Ovarian cancer is the fifth most common cancer affecting women in England and Wales (this includes fallopian and primary peritoneal cancer). Most women are diagnosed at a more advanced stage of the disease and treatment usually involves a combination of surgery and chemotherapy for most women.
This leaflet has been written to help you understand the surgery required for advanced ovarian, fallopian tube or primary peritoneal cancer and to help answer some of the questions that you may have. Cytoreductive or Debulking Surgery is the medical term used to describe this surgery.
On this page
- The surgery
- Consent to treatment
- The health care team
- What are the benefits of the operation?
- Are there any alternatives to the surgery?
- What are the risks of surgery?
- What else might happen as a result of surgery?
- Is there anything I should do to prepare for the operation?
- Useful Numbers
- Website
- Contacts
- Local Support Services
- National Information and Support
- What did you think of your care?
You will be given a separate leaflet called ‘Gynaecological Oncology Surgery – Enhanced Recovery Programme’ which will explain about what to expect when you come in for your surgery and advice for recovery at home.
Your doctor has told you that you have a likely diagnosis (or) confirmed diagnosis of advanced ovarian, fallopian tube or primary peritoneal cancer. Depending on what your CT scan has shown, your doctor may discuss one of the following treatment schedules:
- Surgery (primary surgery) first followed by chemotherapy.
- Chemotherapy (3 cycles) followed by surgery (interval debulking surgery) and then further chemotherapy.
The surgery
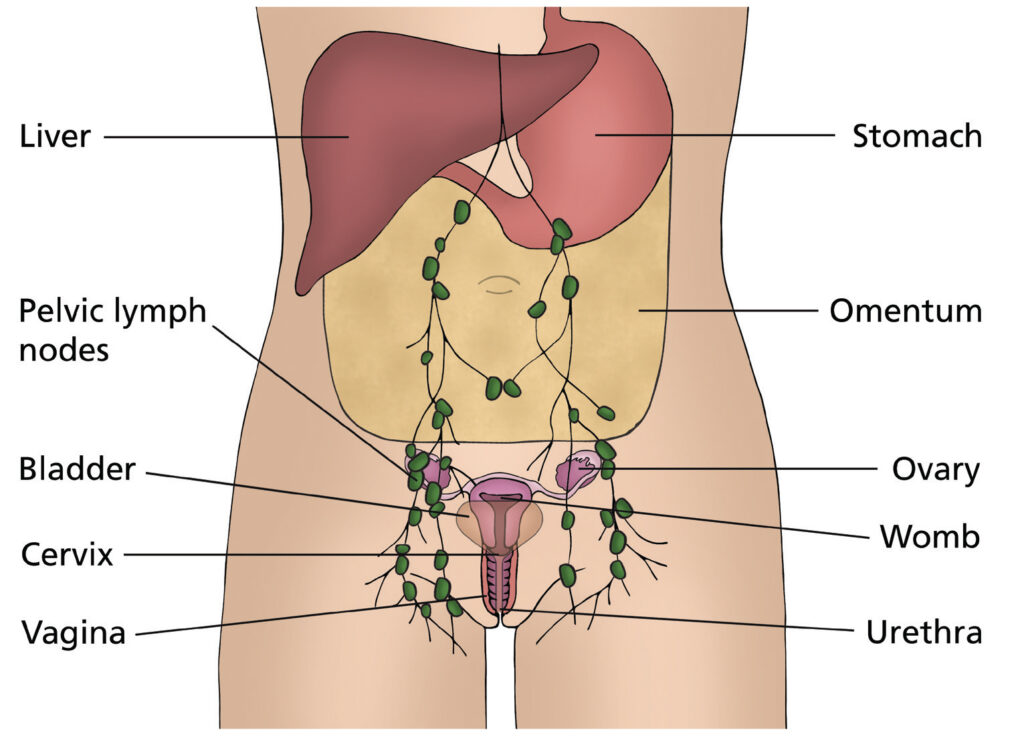
Standard surgery for ovarian cancer usually involves removal of the ovaries and fallopian tubes along with the womb and the omentum (fatty membrane covering the organs inside your tummy). The lymph glands may also be removed if they are found to be enlarged on your CT scan.
Extensive cytoreductive surgery for advanced ovarian, fallopian tube or primary peritoneal cancer is performed with the aim to remove all the visible cancerous tissue from inside your tummy.
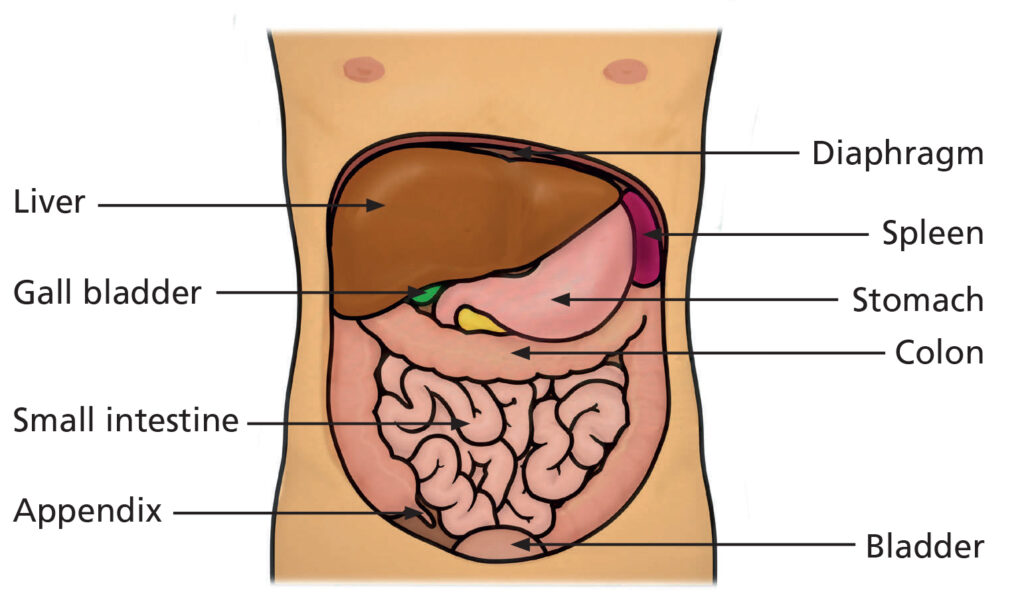
Cytoreductive surgery will involve removal of more tissue when compared to standard surgery. So, in addition to removing the ovaries, fallopian tubes, womb and the omentum, the surgeon may also remove visible cancerous tissue from other organs such as:
- Bowel
- Diaphragm (Muscle layer which separates abdomen from lung cavity)
- Spleen
- Pancreas
- Liver
- Peritoneum (membrane covering the inside of your tummy and internal organs)
- Gall bladder
- Appendix
If you have an area of bowel removed during the operation, the remaining sections of the unaffected bowel may be joined back together if it is safe to do so (this is known as reanastamosis). If this is not possible, the bowel will be diverted to open on the surface of the tummy. This is known as a ‘colostomy’ or ‘stoma’ and allows the stools (faeces) to be collected in a bag attached to your tummy, which can be removed and emptied. This is most likely to be permanent but, in some cases, reversal may be considered. If this is a possibility, it will be explained to you in more detail by your surgeon.
The spleen is an organ in the top left of your abdomen which filters blood and is involved in the immune system to help fight infections. If you have your spleen removed (splenectomy) you will need to have low dose antibiotics every day for life as well as regular vaccinations to reduce your risk of a serious infection. Although the aim is to remove all the visible cancer, sometimes it may not be possible due to disease in certain areas eg bowel surfaces in several areas. In this situation extensive surgery would not be of additional benefit.
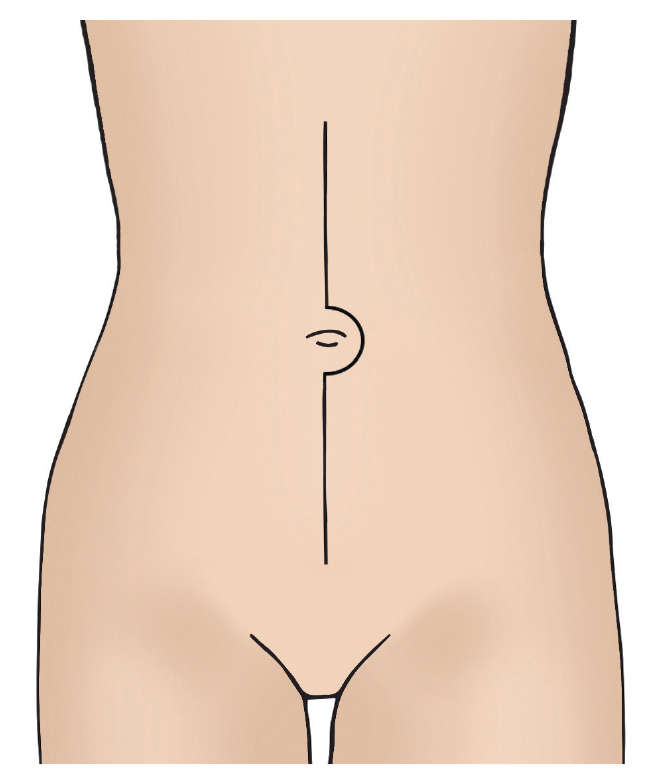
The surgeon will make an ‘up and down cut’ (known as a midline incision) and close the
wound with dissolvable stitches. The area around the scar will feel numb for a while after
the operation but sensation will usually return to it. Occasionally you may have staples which would be removed 10-14 days after surgery.
Consent to treatment
The doctors and nurses will discuss the procedure that has been recommended for you in detail and explain how it will affect you. Once you are satisfied with the explanation and have had all your questions answered, you will be asked to sign a consent form for the operation.
You will also be asked for permission to collect details of your operation to record and review what happens to women who have this operation. You may be asked to complete a quality of life questionnaire before and after treatment.
The health care team
Your surgery will be performed by specialists in gynaecological cancer surgery. Sometimes, other specialists may be involved in your operation such as:
- Gastrointestinal (bowel surgeons)
- Hepatobiliary (surgeons who treat conditions involving the liver, pancreas and spleen)
- Urologists (surgeons who deal with kidneys, bladder and the tubes that carry urine to the bladder)
What are the benefits of the operation?
The benefits of the operation depend on whether the surgeon is able to remove all visible cancer tissue. The aim of the operation will be to remove all visible cancer in order to improve your outcome.
Are there any alternatives to the surgery?
Your health care team will discuss the alternative options which are chemotherapy alone or having no treatment at all. The risks and benefits of all approaches will be discussed with you.
What are the risks of surgery?
There are risks associated with any surgical procedure. Your surgeon will explain these risks to you before you sign your consent form. This form confirms that you agree to have the operation and understand what it involves.
Possible risks and complications are:
- Problems caused by having a general anaesthetic; for example, you may feel sick afterwards. It is also possible to have an allergic reaction, although this is rare. Please tell your doctor about any allergies you have.
- Heavy bleeding during or after the operation; this may need to be treated with a blood transfusion.
- Infection; This would be treated with antibiotics.
- Damage to your bowel, bladder or ureters (the tube that carries urine from the kidneys to the bladder) during surgery – this would be repaired during your operation.
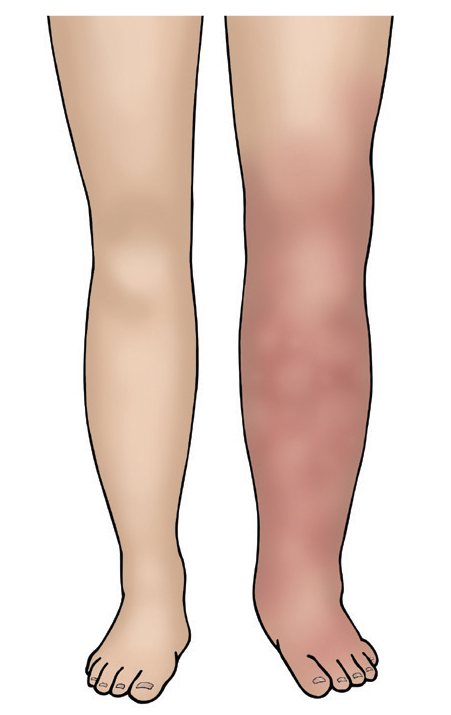
- A blood clot in the leg (deep vein thrombosis) which can sometimes lead to a blood clot in the lungs (pulmonary embolus) – moving around as soon as possible after your operation can help to prevent this. You will be given surgical stockings (known as TEDS) to wear and injections to thin the blood which both help to reduce the risk of blood clots. You may continue to have these injections for up to four weeks.
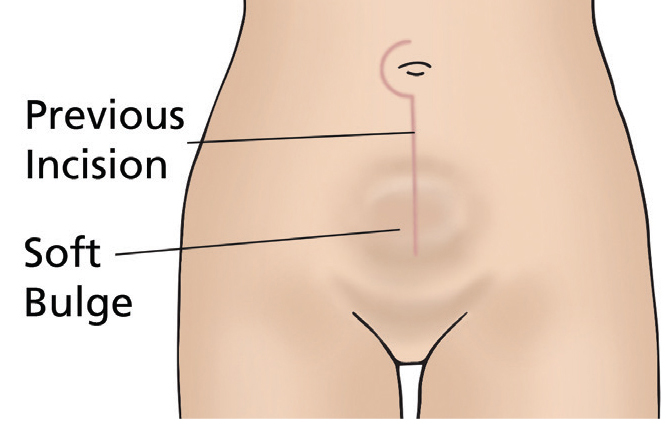
- Incisional hernia; where there is a weakness in the wound allowing tissue or bowel to push through and appear like a bulge. Incisional hernias can develop months or years after surgery and can be repaired by another operation.
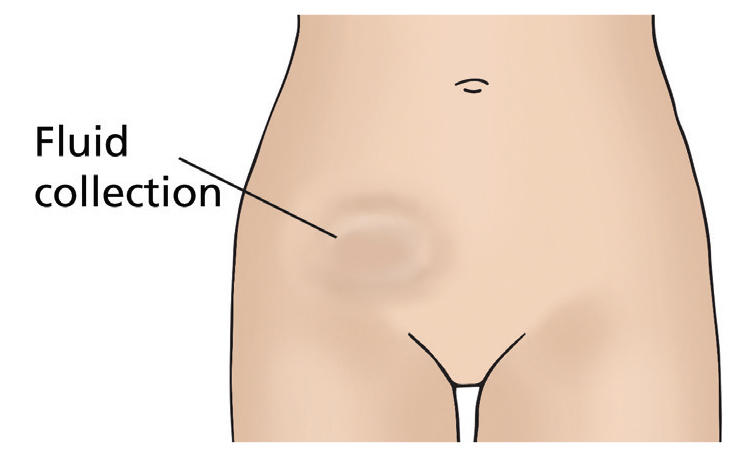
- Lymphocyst; This is a fluid collection at the site where lymph nodes have been removed. The fluid is often naturally reabsorbed by your body but may require draining if large or causing you discomfort.
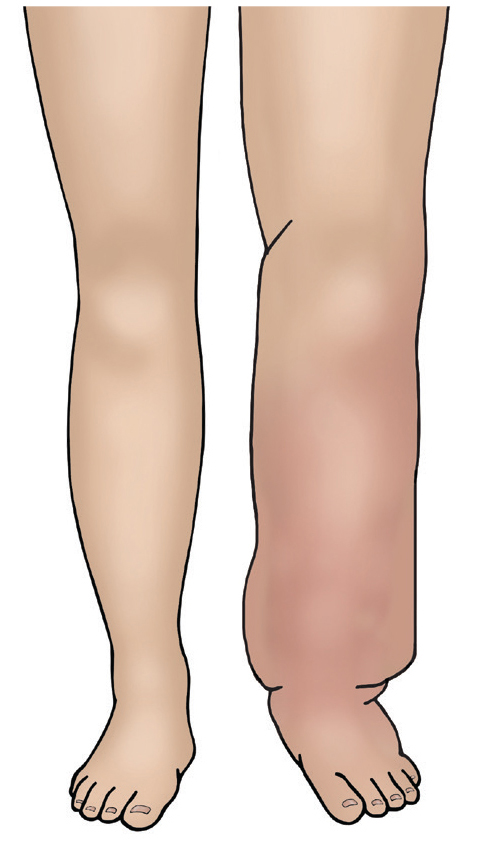
- Lymphoedema; if you have some lymph nodes removed during surgery there is a small risk that in the future your body will find it harder to drain fluid from your legs and lower body. This causes swelling of the legs and lower body known as lymphoedema. If you develop this problem then you can be treated by a lymphoedema specialist. You can discuss this further with your gynaecology specialist nurse or doctor. There is also a booklet you can read that can give you more information.
- A vesicovaginal fistula; is a hole between the bladder and vagina. It allows urine to pass from the bladder to the vagina.
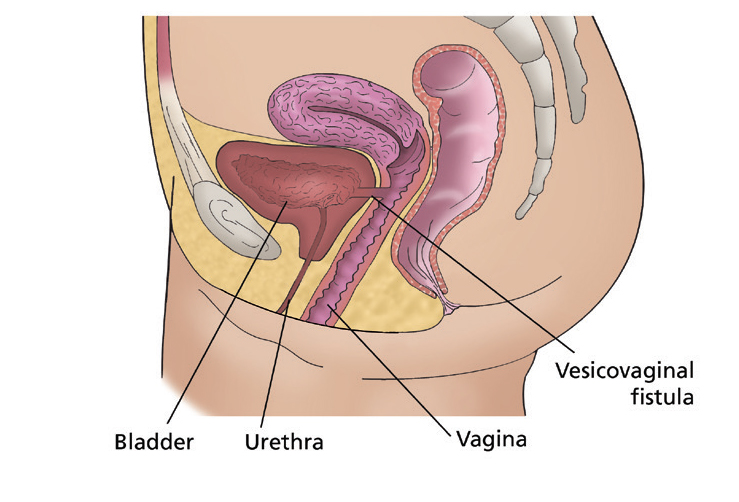
- A rectovaginal fistula is a hole between the rectum and the vagina. It allows faeces to pass from the rectum to the vagina.
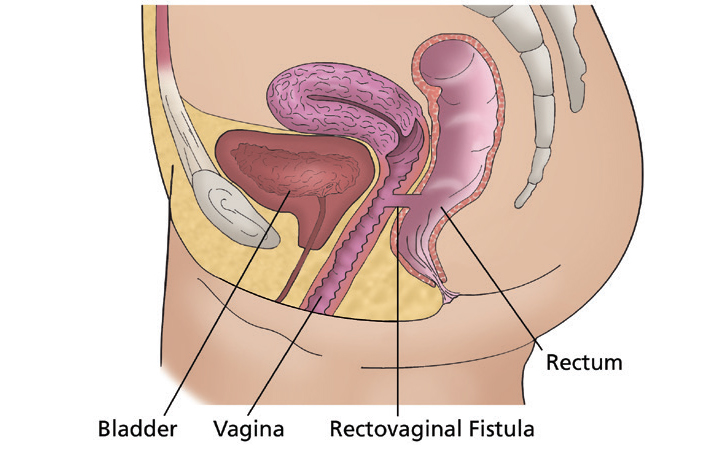
- Fistulas can be repaired but sometimes it will involve another operation.
- A build up of fluid around the lungs, which would have to be drained.
- Fluid leaking from the pancreas which would have to be drained.
- Air collecting in the chest cavity which may cause the lungs to collapse.
- The risk of death is approximately 1%.
What else might happen as a result of surgery?
As mentioned earlier, your surgery may result in the formation of a colostomy (stoma).
Your surgeon may request a colorectal nurse specialist to see you before your operation. The nurse will mark the area of your tummy where a potential stoma could be formed. They will also provide education and emotional support.
If a stoma is formed during your surgery, you will be supported on the ward to help you become confident with caring for your stoma. Once discharged home you will have access to a community stoma nurse specialist team. The possibility of having a stoma can worry many patients. Please talk through your concerns with your surgeon or clinical nurse specialist team, who can support you with any decisions.
Your bladder may take some time to begin working properly again. Some women have a loss of feeling in their bladder and therefore do not know when their bladder is full. This may take some time to return to normal. During this time you need to go to the toilet regularly to empty your bladder.
Some women find that their urine stream is slower so it may take longer to pass urine. This usually improves as your body recovers from surgery. Rocking gently backwards and forwards or side to side whilst sat on the toilet can help to fully empty your bladder.
Your bowels may take some time to begin working properly again. Some women have a sluggish bowel for a number of days after surgery which can cause you to feel sick until it starts to work again. If this happens then you will be advised to walk around the ward as much as possible to stimulate your bowels to work.
This can be difficult if you are feeling unwell but it is important to do so to speed up your recovery. We will also give you anti-sickness medication. Passing wind is a good sign that your bowels are starting to work.
Trapped wind and wind pain is very common after surgery. Walking around as much as possible can help relieve this. You may find that peppermint tea and/or peppermint capsules helpful which are both available on the ward. Wind usually starts to improve once you are having your bowels opened.
Visit our website where you will find patient information leaflets and videos related to your surgery
Is there anything I should do to prepare for the operation?
Make sure that all of your questions have been answered and that you fully understand what is going to happen. If you have any questions after you have left the clinic, you can contact the nurse specialists who will be able to help you. (Scroll down to contact numbers).
You are welcome to visit the ward and meet the staff before you are admitted to hospital – ask your specialist nurse or pre- assessment nurse to arrange this.
You should eat a balanced diet, and if you feel well enough, take some gentle exercise before the operation, as this will also help your recovery afterwards. Your GP, practice nurse or the doctors and nurses at the hospital will be able to give you further advice about this.
Before you come into hospital for your operation, try to organise things for when you come home. If you have a freezer, stock it with easy to prepare food.
Arrange for relatives and friends to do your heavy work (such as changing your bedding, vacuuming and gardening) and to look after your children, or other dependants if necessary. Arrange for somebody to take you home from hospital when you are discharged. If you think you may have problems coping at home, you can discuss this with the nurses on the ward.
After the operation
After the operation, you will be cared for in the recovery unit in theatre for monitoring. You may then be transferred to the high dependency unit (HDU) or intensive care unit (ITU). Your stay in the HDU may vary between overnight to a few days.
You will have a drip in your arm so that we can give you fluids and pain relief after the operation. This will be removed when you are able to eat and drink.
You will have a tube in your bladder (catheter) to allow the urine to drain. This allows us to monitor how well your kidneys are working. This is usually removed when you are able to walk to the toilet to pass urine.
Some women will have a drain (small plastic tube) placed near their wound to remove blood or other fluid, preventing it from building up in the body. This is usually removed after a few days.
Occasionally, there may be a tube in your nose (nasogastric/NG tube also called a rhyles tube) to drain the fluid in your stomach and stop you from feeling sick. You will be able to talk and breathe while the tube is in. It will be removed once you are able to drink without being sick.
Very rarely, some women may need to be given a feed through a drip in the neck or their arm. This is called total parenteral nutrition (TPN). If you need this, you will be monitored everyday by the nutrition team. You will be reviewed daily by your team of doctors and nurses. You will see a physiotherapist who will help you with breathing/coughing and movement exercises.
If you have a stoma, you will be seen by the stoma nurses, who will teach you how to become independent with emptying and changing your bag.
When can I go home?
You will usually be able to go home around 10 – 14 days after your operation. This depends on your individual recovery, how you feel physically and emotionally and the support available at home. If you require hospital transport for your discharge home, please let a member of staff know in advance.
Follow up
Your GP will be informed of your discharge from hospital. You will be seen in the outpatient clinic 2-3 weeks later with the tissue results (histology) from surgery. You will also be given an appointment to see the chemotherapy specialists (medical oncologists) to discuss further treatment.
Psychological support and counselling
You may find you are having difficulty coming to terms with your illness and the effects of your treatment and/or surgery. As part of your care, your team will discuss these issues or concerns with you. If required, your team may refer you to a trained counsellor with your consent. Your clinical nurse specialist will advise you of local support available in your area. You may also find it helpful to contact national support groups/charities which are listed at the end of this booklet.
What happens if I have any problems after I’m discharged home?
If you have any problems or have any questions after discharge, you can contact your key worker/clinical nurse specialists who will advise you or arrange for you to be seen. Alternatively, you can contact ward J98 for advice.
Useful Numbers
For queries regarding your admission please call the relevant secretary.
For advice on any medicines you have received from the hospital call:
Website
On this website you will find information about our team, what we do, information leaflets and videos
Contacts
For advice please call your Clinical Nurse Specialist (CNS) or Ward J98
If your nurse specialist is not available then please leave a message on the answering machine and they will ring you back. Please note this may not always be the same day.
In an EMERGENCY please attend your nearest Accident and Emergency Department.