This information leaflet has some very important information about Spinal Cord Stimulators (SCS) and it is essential that you read and understand all this information before having an SCS implanted. If you have any questions, please discuss these further with the team (contact information included in this leaflet).
What is Spinal Cord Stimulation?
Spinal Cord Stimulation (SCS) is stimulation of the spinal cord by tiny electrical impulses. SCS works by delivering low power electrical stimulation to the spinal cord masking the sensation of pain. SCS systems can be easily and painlessly programmed to best manage your pain. It is used for chronic (‘long term’) neuropathic (‘nerve’) pain. It is often used when other treatments such as medication, physiotherapy or injections haven’t worked.
Although SCS may allow you to reduce some of your medications it can still be used alongside them. It can be seen as a ‘tool’ to allow you to revisit treatment options that may have not worked in the past such as exercise or physiotherapy. It may reduce your pain but it will not take it all away.
In the event that you no longer require SCS, the device can be removed.
How does SCS work?
When you have pain, pain signals are transmitted up the spinal cord to your brain. SCS is the stimulation of the nerves around your spinal cord by tiny electrical impulses. The electrical impulses then block these pain signals from reaching your brain. The electrical impulses are delivered through a lead, which is implanted near your spinal cord. The lead is a flexible insulated wire, which is powered by an implanted battery (Internal Pulse Generator or IPG).
You may experience tingling in the area where your pain is, but in most types of SCS no sensations are felt when the device is switched on.
The stimulation can be adjusted in terms of strength and area of coverage via an external programming device, by either a nurse from the Pain Team or a representative from the SCS Company. You may also be able to make some changes to the stimulation yourself by using your own programmer.
The implantable system does not make any noise. The battery (IPG) may be felt, and occasionally seen as a small bulge under your skin, but does not normally show through your clothes.
Will SCS work for me?
Unfortunately Spinal Cord Stimulators do not work for everyone. There is approximately a 60-80% chance of an SCS providing you with on average a 50% reduction in pain. This also means that there is around a 20-40% chance it will not work for you. Spinal Cord Stimulators will only work for neuropathic (nerve) pain.
Your Consultant will have already assessed some or all of your pain as being neuropathic. However, some patients have “mixed” pain. By this we mean you may have some mechanical pain, for example joint, muscular or arthritic pain or pain from other conditions such as fibromyalgia.
The SCS will not help with these types of pain.
Equipment Overview – Fully Implanted System
The fully implanted SCS system consists of an implanted lead and an implanted battery. You may also have an anchor which holds the bottom of the lead in place.
You will have your own external patient programmer to allow you to adjust your SCS at home. You may also have a recharger to charge the implanted battery. Any decisions as to which type of SCS you are suitable for will be based on your type of pain and clinical need and will be decided in our multidisciplinary team meeting (MDT). A representative from the SCS Company may see you on the ward after your implant to show you how to use your equipment.
But sometimes this is not done on the day of implant and a separate appointment will be made for you for this to be done.
*Please note
The images in this leaflet may not represent the SCS equipment for your particular system and are just examples. Each type of SCS will look different and may have different components.
Internal Components
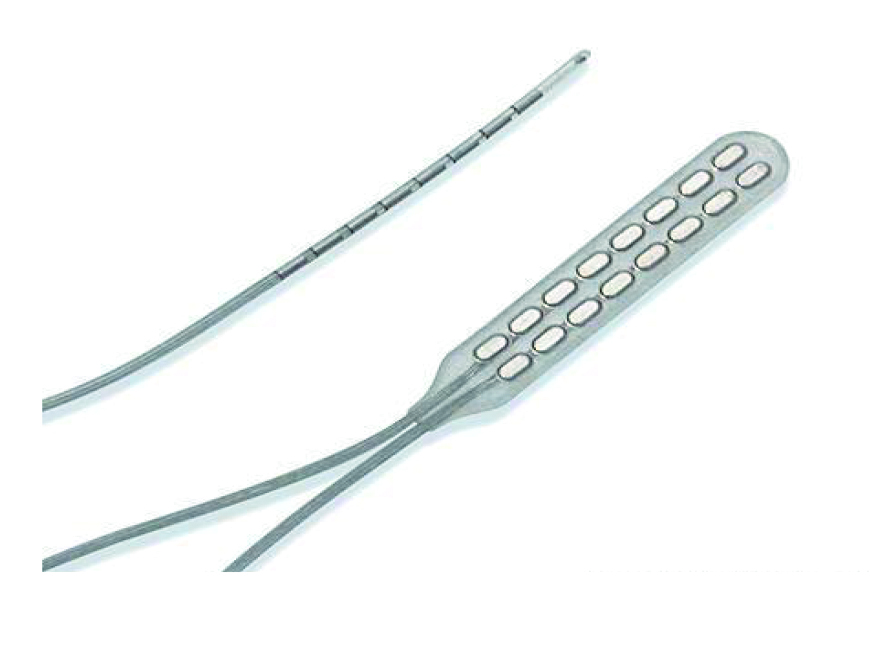
Lead/Electrode
SCS leads are special insulated wires designed to deliver electrical stimulation to the spinal cord. Most spinal cord stimulators use 1 lead but sometimes 2 may be used. This will usually depend on the area of your pain, and your Consultant or nurse will discuss this with you. The lead is usually 20 inches (50 cm) long and is placed under the skin near your spine. At the end of the lead is a set of electrodes (small metal plates) through which the electrical stimulation is delivered to the spinal cord. By activating these electrodes we are able to deliver the electrical impulses to your spinal cord, this is what we refer to as a ‘program’.
In selected cases we place a flat lead by making a larger surgical incision. This is a more invasive operation done by our Neurosurgeons and you will be given further information if you need this for clinical reasons.
Battery/Internal Pulse Generator (IPG)
The battery is a small metal box implanted under your skin which powers the electrodes and controls the stimulation. It is programmed by the nurses in clinic and controlled by your patient programmer.
Your battery may be slightly visible through your skin and it may be several weeks after your implant before any discomfort around this area settles down.

External Components
Programmer used in clinic
The programmer (which may look like a handheld device or a laptop) allows the Pain Nurse to adjust your SCS and provide you with some programs to try at home to see if they are helpful for your pain. The programmer is placed near to or over the area where your battery is implanted so you will normally need to be in clinic to have your SCS checked or adjusted. Our programmer communicates with your IPG. The patient programmer can help us to identify which programs you have tried, how long they were used, and if you had any issues with charging of the stimulator, or if it had been accidentally switched off.
With some SCS we may be able to program the stimulator remotely, this means you may not have to come to the hospital to have your stimulator reprogrammed. This is only for some types of stimulator and if applicable the team will discuss this with you further.
Patient Programmer
You will be given a patient programmer to take home. You may be shown how to use this by the SCS company representative before you leave hospital. But this may be done at a separate appointment. This allows you to alter your stimulator within pre-set parameters. You can use the patient programmer to switch your system on and off. You may also be able to use it to check the battery level and to check or change which program you are on (if necessary). Your patient programmer may run on ordinary batteries or may need to be recharged at the mains like a mobile phone. If you are unsure how to use your patient programmer please refer to the information you are given after your implant. If you are still having difficulties, please call the Pain Nurses for further advice.

Recharger
Some IPGs need to be recharged and some do not. If you have a rechargeable SCS you may be given a recharger before you leave hospital or at a separate appointment. The recharger itself will need to be charged by plugging it in at the mains. A company representative or Nurse Specialist will explain how to do this and they will also explain how often you need to charge as this can be daily or weekly depending on which type of SCS you have. Please only use the equipment given to you to recharge your IPG.

Do not use any adaptors or in-car chargers. If you are unsure how to use your recharger please refer to the information you are given after your implant. If you are still having difficulties, please call the Pain Nurses for further advice.
In the first few days or weeks after your implant recharging your IPG may be tricky as there may be some post-op swelling and discomfort around your wound. This is normal and will settle in the coming weeks. If you are having difficulties, please call the pain nurses for further advice.
SCS Trial
In order to have a spinal cord stimulator implanted, some patients may first have a trial. The trial procedure consists of a short test stimulation period (usually for one to two weeks) before having the full implant.
If you have a trial, the lead(s) are implanted in an operating theatre. On the day of your implant you will be asked to change into a gown and you may be asked to fast (not have anything to eat or drink). This is usually done as a day case using local anaesthetic, painkillers and some light sedation and you can usually go home the same day. During the procedure you will usually be asked to lie on your front and you may have a cannula (small plastic tube) inserted in the back of your hand or arm and an oxygen mask if necessary. Your doctor will inject some local anaesthetic in your back before making a very small incision to place a lead close to your spinal cord. The theatre staff are there to support you so please let them know if you have any questions or feel anxious. There may also be a Company Representative from your SCS Company in theatre with you. The lead placement is one of the keys to successful results with SCS.
For some types of SCS the lead placement is a standard procedure and is always placed in the same area of your back. For other types you may be asked if you can feel any stimulation in the area of your pain and the lead may be moved along your spine accordingly. In this case your involvement is very important, so you should tell the doctor exactly how the stimulation feels. Do not be afraid to be truthful, as it may be important to make sure that the stimulation is in the correct area for your pain.
During the trial, the end of the lead remains on the outside of your body and is secured to your back with a dressing. It is then attached to an extension lead which connects to a power pack which powers the lead. This power pack may be under another dressing which is taped to your back or it may be a larger power pack which is attached to a belt that you wear around your waist.
After around 10-14 days you will then return to clinic to be assessed by a Clinical Nurse Specialist, who will discuss with you any improvements in your pain and quality of life. Your external trial leads will then be removed in clinic. This is usually a quick, painless procedure and you do not need any injections or anaesthetic. It is important that you are open and honest about the results of your trial as any pain relief you achieve from a permanent system is not likely to be any better than a trial. There are also occasions when the full implant does not give you as good pain relief as during the trial.
Sometimes tests are done on the day in theatre to check the lead(s) are in the right place and you may be asked some questions regarding the feeling of the stimulation and the area of your pain. Occasionally the trial may last longer than one to two weeks but this will be discussed with you and appointments made where required.
Implant Procedure
A full permanent SCS may be implanted if you have had either a successful external trial or a successful on-the-table trial. Alternatively, we may proceed straight to a permanent system. The full system involves having both the lead and IPG implanted. The decision will be made on an individual patient basis.
This is usually done as a day case using local anaesthetic, painkillers and some light sedation and you can usually go home the same day.
During the surgical procedure, an incision is made over the spine so that your doctor can implant, position and secure the lead into your back, much the same as for the trial (refer to trial section above) but in this case instead of exiting the body, the lead will then be connected to the internal IPG/battery under the skin.
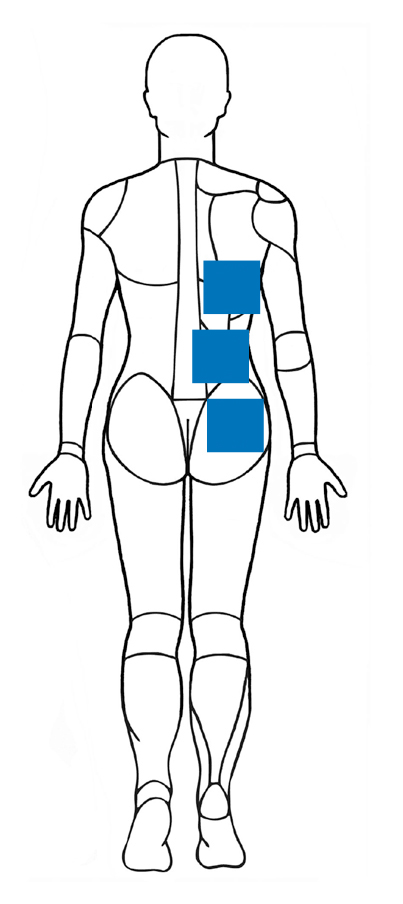
To implant the IPG, your doctor will form a pocket under your skin (usually above your buttock or below your ribs) that is large enough to hold the IPG. At this point during the surgery you may be given some more painkillers and/or some light sedation to keep you comfortable. Once the lead is connected to the IPG, the incisions are stitched and/or glued and the surgery is complete. You will then be taken to either the post-anaesthetic recovery unit or to the ward.
Placement of IPG/battery
The IPG/battery is usually placed under the skin on the chest wall or just above your buttocks on either the left or right side. Your Consultant will discuss battery placement with you prior to surgery. It is important that you consider things such as how you sleep at night (i.e. if you always sleep on one side) and clothing that you wear (e.g. bras and belts) when discussing battery positions with your doctor.
After the Procedure
After the procedure, a Company Representative may visit you on the ward and switch the stimulator on. At this point you may have some programs installed to try at home. You will be shown how to use equipment such as your patient handset and if applicable, your recharger. Sometimes this will not be done on the day of implant and a separate appointment will be made for you for this to be done.
You are likely to experience some pain or discomfort around the wounds in your back for a few days after your procedure. Your battery site may be uncomfortable for several weeks. Your GP can prescribe some painkillers to help with this pain if necessary.
It is important you check your wounds daily for any signs of infection or ask a friend or relative to do this for you. Some swelling around your battery site is normal but if you have any sudden swelling, pain or redness or leaking blood or pus from either of your wounds please refer to the written discharge advice you have been given and seek medical advice.
Important
It is essential you also contact the Pain Nurses to let them know if you have any problems with your wounds. If you have any concerns with your wounds it is very important to get them reviewed on the same day. If you cannot speak with a Pain Nurse, then please ensure you seek alternative medical advice straight away, such as your GP Practice or A&E if urgent attention is needed.
We do ask you to avoid certain activities during your external trial and for several weeks after your permanent system is implanted, for example, bending, lifting, twisting and driving.
However, it is important to try and maintain your normal activity level after the stimulator is implanted.
Reprogramming
You may have several programs on your SCS when you leave hospital. However, it is likely your programs will not be altered in the first six weeks after your procedure. This is because it takes time for the lead to become settled in place and tissue swelling and pain post-operatively in the first few weeks can affect stimulation and make it difficult to gauge how helpful a program is for your pain. During this time you will have appointments with the Pain Nurses, these may be telephone reviews or reviews via video link.
Sometimes the stimulator is set to give a tingling sensation whilst it is switched on. Other programs are set so that you cannot feel any stimulation. Please check with the nurses or company representative as to which type of program you have.
If you have been told that you have a program that you should not be able to feel and you can feel any ‘tingling’ or any different or new sensations (different to ‘normal’), you should use your patient programmer to switch the stimulator down. This may be caused by overstimulation and this is important as overstimulation can aggravate your pain and make it worse. If you do not know how to do this, or have any concerns, please ring the pain nurses for advice.
If, after 6 weeks your wounds are well healed and you are feeling able to, you can begin to work your way through your programs as instructed by your SCS Company Representative. If you need any help with this please call the pain nurses.
We run face to face clinics for reprogramming and reviewing your SCS but these are on set days, times and locations.
It is important that you understand before having your SCS implanted that although we try to be flexible, we are limited and you will not be able to specify days, times and locations to have your appointments. If you have any concerns with regards to this, please speak to one of the team.
Additional information
Magnets:
Your SCS can be turned on and off by close contact with magnets. This is a safety feature, however other magnets such as those on bags and wallets, children’s toys etc may all turn your SCS off unexpectedly.
Surgery with an SCS:
If you require other surgery once you have had an SCS implanted, there may be certain precautions that your Surgeon may need to consider, for example some of the equipment used during surgery (e.g. diathermy) may be restricted and your SCS may need to be switched off during the procedure. It is important that you let the team carrying out the surgery know in advance that you have an SCS implanted. You can contact the Pain Team for further advice.
MRI scans:
Due to the metal components of an SCS, there are restrictions with regards to having MRI scans. You will not be able to have an MRI while you have a trial. If you are told that you need an MRI and you have an SCS implanted, please make sure the referring person and MRI Department are aware you have an SCS prior to the date of the MRI.
Checks will need to be made prior to the MRI scan being booked and there may be certain things that are needed on the day (i.e. There may need to be a Representative from your SCS company or Pain Nurse there and the system may need to be checked and switched off or into MRI mode prior to the scan). There are also some types of SCS where by you cannot have an MRI scan at all. If you require routine MRI scans, it is important that you let the team know before you have an SCS implanted.
Alarms/airports:
Once you have your permanent system implanted you will be given a card to show to airport staff to say that you have an implanted medical device. This means they may be able to make alternative arrangements with regards to metal detectors. We advise that you keep your patient programmer in your hand luggage so you can check or adjust your SCS during your journey.
Significant, unavoidable or frequently occurring risks
There are risks and complications with having an SCS. The serious risks are rare.
Risks include:
- Failure of SCS to provide pain relief.
- Allergy to implant materials.
- Bleeding in your back or at battery site (including risk of paralysis).
- Leaking of spinal fluid causing a headache.
- Infection at the lead or battery site (including risk of meningitis and paralysis).
- Retained implant components – you may have damage to some of the stimulator which cannot be safely removed.
- Need for revision surgery (to have lead &/or battery replaced).
- Bruising and pain where the operation has been performed.
- Nerve damage.
- Work and hobbies – It is important to discuss your work and hobbies with the team as some jobs (such as welding or if you work close to strong magnets) or activities such as contact sports may not be advisable if you have an SCS implanted.
There also may be restrictions with activities such as deep sea diving, if you dive, please ask advice before having an SCS implanted.
These will all be discussed in more detail at your information session with the pain nurses and with your Consultant. If you have any queries with regards to the risks, please discuss it further with the team.
What happens next?
After you have had your Information Session your case will be discussed in our multidisciplinary team meeting. From here, if you are deemed suitable for an SCS you will be added to our waiting list, waiting times may vary. You will then have an appointment with a pre-assessment nurse and one last appointment with your Consultant, which may be over the telephone. This will give you the opportunity to ask any questions or discuss any concerns you may have.
- If you have already had your Information Session, we hope you have found it useful and informative.
- If you have not, you will need to have an Information Session with the pain nurses and this may be face to face or via video link.
- It is very important that you understand about the risks and benefits of SCS and about what having an SCS involves.
Alternatively, there is further information available on our website. You will also have the opportunity to ask your Consultant any questions during your final check appointment and you will receive an appointment letter through the post for this.
Contact us
When you go home it is important that if you experience any of the following signs/symptoms
- Redness, pus, tenderness or excessive swelling or pain at any of your wounds.
- Feeling generally unwell with a high temperature or flu like symptoms despite the fact that all seems to be well with the surgical wound.
- High temperature, neck stiffness, headache.
- Numbness and /or weakness in your arms or legs/ inability to weight bear.
- Difficulty passing water/incontinence of faeces.
Please note
You will need to attend the Leeds General Infirmary Accident & Emergency Department to be assessed by the Neurosurgeons or the nearest Accident & Emergency Department that has Spinal/ Neurosurgeons based at that hospital.
Take this leaflet with you, the Doctors there can always contact the on-call Chronic Pain Consultant for advice if required.
IMPORTANT – These problems may happen any time after your operation.
Please also contact the pain nurse specialists as well as seeking medical advice in Accident & Emergency.
Instructions for patients with spinal cord stimulators (SCS) following their operation
For 6 to 8 weeks after your operation the stimulator lead can easily move/ become displaced. As a consequence it is important you limit your activity by following the precautions below. This helps reduce the risk of the lead moving which can result in loss of stimulation to the painful area.
Immediately after your operation
- Ask the nurse when you can get up and out of bed, do not attempt this alone the first time.
- If your wound leaks excessively inform the ward nurses.
For 6 to 8 weeks following the operation
Try to avoid
- Raising your arms over your head.
- Bending, lifting heavy loads and twisting
- Sitting or lying for long periods.
- For at least 4 weeks after your implant and during the trial do not drive (or according to your doctor’s instructions). Driving can cause you to move abruptly or shift in position, which increases the risk of the lead moving.
- If you have a ‘tingly’ program or any program you can feel, you must not drive with your stimulator switch on.
Do
- Contact the Nurse Specialists if there are any signs of infection to your wounds. If you are unable to speak to one of the Nurse Specialists, please seek alternative medical advice from GP or A&E if urgent.
- Lie straight in bed (if possible) use pillows if necessary for support.
- Sleep on a firm mattress which supports you.
- Obtain approval from your pain doctor before seeing a chiropractor or osteopath (manipulation may move the position of the lead.)
- Move your body without twisting by moving your shoulders and hips at the same time with a ‘log-rolling’ movement. Please ask the nursing staff if you need further explanation of how to do this.
- Build up your physical strength by walking for brief periods of time each day and gradually increasing distance.