This leaflet aims to help you and your family understand more about radiotherapy to the brain.
This is in addition to the information you will receive from your clinical oncologist (who is a specialist doctor in cancer treatment). Their team will be caring for you during your treatment. This team will include radiographers and clinical nurse specialists, but may also include social workers, physiotherapists, occupational therapists and dietitians.
This leaflet describes radiotherapy planning and treatment. It also explains the side-effects which you may experience during and after treatment.
Each person’s treatment will vary, so the information given is a general guide. The healthcare team looking after you will explain your treatment and the side-effects in detail. If you have any questions after reading this leaflet, please speak to the team looking after you or ring the numbers at the end of the leaflet.
Staff will make every effort to meet your individual needs or will direct you to the person who can help.
Please do not bring any valuables into hospital with you as the Trust cannot accept liability for loss or theft.
What is radiotherapy?
Radiotherapy is the use of high energy X-rays and other types of radiation, to treat cancer. The radiotherapy causes damage to the cancer cells in the treated area. Although normal cells are also affected, they can repair themselves and are able to recover.
Radiotherapy is a local treatment. This means it only affects the part of the body that is treated. It may be used as the main treatment for a brain tumour, or as an addition to surgery. When you are having your radiotherapy you do not feel anything and it does not make you radioactive. You may hear a buzzing noise when the machine is switched on. It is perfectly safe for you to be around others, including children and anyone who may be pregnant, throughout your treatment. Your treatment will usually be given as an outpatient.
You will have your radiotherapy on a treatment machine called a Linear Accelerator as shown below in the photograph.

Who will I meet?
Therapeutic Radiographer
Radiotherapy is given by therapeutic radiographers of any gender, who are highly trained in the accurate planning and delivery of radiotherapy treatment. You will see your radiographers at each treatment session and they will be happy to answer any questions you may have.
Students
The radiotherapy department is a training centre for therapeutic radiographers. They are supervised at all times. If you do not wish students to be present, please speak to a member of staff. This will not affect your treatment or care.
Others involved in your care
You may meet other staff whilst you are coming for radiotherapy. Everyone you meet will introduce themselves, tell you their job title and explain the role they have in your care.
Important advice before your treatment
Pregnancy
It is important that patients of child bearing potential are not pregnant at the start of a course of radiotherapy and that they do not become pregnant during a course of radiotherapy, because it can have an effect on the unborn child. Use an effective form of contraception for example condoms, coil, depo injection, or contraceptive pill.
For more information see the ‘Contraception and pregnancy during cancer treatment’ leaflet. Please do not hesitate to ask your doctor or nurse if you have any questions or concerns about these issues.
Planning your treatment
Your first appointment may be in the Planning Clinic or
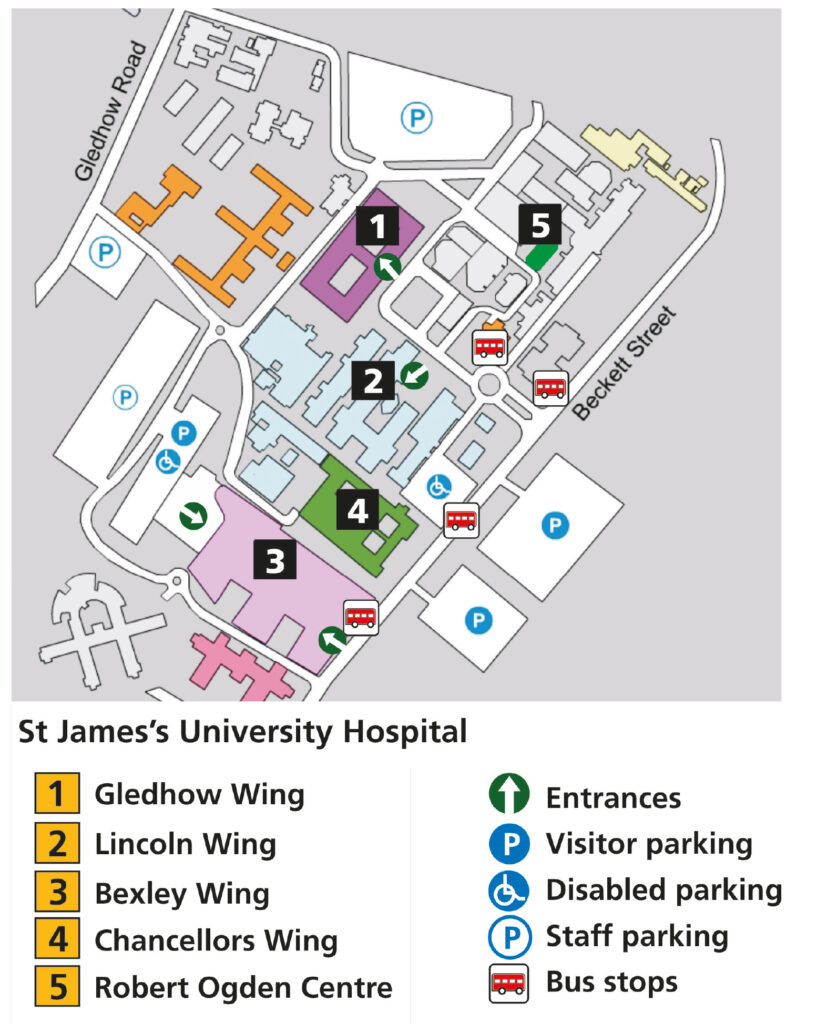
Level 1 Outpatients in the Bexley Wing. We will contact you by phone, with an appointment for your radiotherapy planning session. Some tests and scans may be needed to help plan your treatment. We will explain which of these you will need when your appointment is made. Directions to the hospital and transport arrangements will be discussed with you at this point. You will see your clinical oncologist or a member of their team where they will discuss your treatment with you. You will be asked to sign a form giving your consent to treatment.
What to bring with you
- a list of all questions you may have;
- an up-to-date list of all the medications you are taking (including inhalers, sprays, vitamins or herbal products);
- something to eat and drink and something to keep you occupied as this first visit can be quite lengthy (up to two hours)
Mould Room
Radiotherapy involves exact positioning of the radiation beam, so you will need to stay very still while you are having treatment. To help you stay still when treating the head, we will make a mask for your head (shown here in the picture). You will wear your mask for your planning scan and treatments.

For the mask you will be given an appointment to attend the Mould Room where the masks are made. If you have any concerns about the mask, please let your clinical oncologist or a member of their team know. We have a support team who will help you.
Your Planning scan
You will need to have a Planning CT scan as part of the planning process. This is done on a machine called a CT Scanner, shown here in the photograph. It allows the images from the scan to be sent to the radiotherapy computer planning system. You will need to wear your mask for this scan.

You may also need an MRI scan (please see photograph below), again for planning purposes. This involves a separate appointment in our department. This could take place the same day as the CT scan, or may be on a different day.

Your radiotherapy is individually planned by your oncologist and a specialist physics team using information from the CT and MRI scans. This can take up to a few weeks if it is a complex treatment. When you attend for your planning visit you will be given information on when the treatment is expected to start.
Contrast (dye)
A special contrast agent, often called a dye, may be used for your scan to make specific organs, blood vessels and/or tissue types ‘stand out’. This can make it easier for the doctor to plan your treatment.
The dye is given through a very small plastic tube called a ‘cannula’ into a vein in your arm. You should tell the radiographer if you have any allergies, but they will go over this before they use any dye.
Contrast side-effects
You may notice a warm feeling throughout your body and have a metallic taste in your mouth. You may also feel as if you have passed urine (had a wee). This will pass very quickly. There is a slight risk of an allergic reaction to the injection, such as a skin rash. However, it is very rare that such reactions lead to other complications.
The staff in the radiotherapy department are highly trained to manage any complications and again the risk involved is very small.
Following the scan the radiographers will give you the time of your first appointment on the treatment machine. This is most likely to be a couple of weeks after the planning visit.
The radiographers will talk to you about any further appointments you have.
Having your treatment
When you arrive for your treatment you should go to the main radiotherapy reception desk at the entrance of the radiotherapy department. On the first occasion you will be given all your appointments and be escorted to the waiting area for your machine.
Treatment is given on a machine called a Linear Accelerator, shown here in the picture.

Treatment is normally given daily, Monday to Friday, however your treatment may start on any day of the week.
Whenever possible you will be treated at the time of day that suits you, but this cannot always be arranged or guaranteed. There may be occasions when you may have a longer stay in the department or be asked to attend at a different time. This is for example to see your oncologist or nurse specialist.
You can expect to spend 10-15 minutes each day in the treatment room. The treatment machine is only switched on for a fraction of this time.
For most of the time the radiographers are carefully placing you and the machine in the correct position for your treatment. The machine does not actually touch you. You will also hear the radiographers giving each other instructions and information relating to your treatment. It is important to stay as still as possible and breathe normally.
Once you are in the correct position the radiographers will leave the room to switch on the machine. You will only be alone for a few moments at a time. The radiographers will be watching you on a closed circuit TV monitor as shown here in the picture. The CCTV camera is not recording or saving any images.

There is also an intercom system so the radiographers can talk to you.
If you would like to listen to music during your treatment please let us know.
Although you have to lie still, you can breathe normally during your treatment. The radiographers may need to come in and out part way through each treatment. The machine stops automatically after your prescribed dose of treatment has been given. The machine can also be stopped at any time if required. The treatment machines make a buzzing sound when they are switched on. You do not feel anything. For the first few treatments and also intermittently during treatment we will also take images to check the accuracy of the treatment. This will take a few more minutes.
These images do not monitor your condition but are purely for treatment accuracy.
After the treatment is complete the radiographers will come back into the room and help you off the couch.
During the treatment course, please tell the radiographers how you are feeling. If you have any problems or questions, please let them know. Your Clinical Nurse Specialist (CNS) will see you once a week in the Princess Royal Suite, also situated in the department, to see how you are getting on. They are in close contact with your clinical oncologist and will monitor any side-effects you may be experiencing. You can expect to be in the department longer than usual on this day.
Some days the Radiotherapy Department may be very busy and your appointment time may be delayed. We will keep you informed of any delays. Please look out for delay signs displayed in waiting rooms.
Your treatments will generally be on the same machine, although there may be days when this machine is being serviced and your treatment will be in a different room.
Your appointments for Radiotherapy may not all be at the same time each day and may need to change. It is also possible that during your course of treatment you may miss a day’s treatment due to machine maintenance or bank holidays. It is therefore important to speak to a health care professional before booking a holiday immediately following your radiotherapy.
For appointment queries please telephone the number on your appointment letter for further advice.
Driving
Your brain may be affected by either your disease or your treatment, and therefore you MUST NOT DRIVE. Your doctor will be able to provide further information about this restriction if this applies to you.
Important
If you experience any of the following problems before starting, during or after your course of radiotherapy, please report them immediately to a radiographer, nurse or doctor. These symptoms may require changes in your medication or treatment schedule.
- A change in vision, hearing or speech.
- A change in sensation of the face, body, arms, legs.
- An abrupt change of bowel or bladder habit.
- Weakness.
- Unsteadiness.
- Dizziness.
- Seizures – ‘fits’ or ‘blackouts’.
- Severe headaches and vomiting.
Research at Leeds Cancer Centre
Leeds Cancer Centre is a major centre for cancer research. You may be asked if you would like to help with some of the clinical studies. You are under no obligation to take part in any trials, and your treatment will not be affected in any way if you do not wish to take part. If you do take part in a clinical trial you may meet a research nurse or radiographer who will be helping to run the trial.
Side-effects
The type and extent to which you may experience these side effects is individual. It depends upon many factors such as the position and dose of your treatment. It is important to remember that not everyone experiences these side-effects.
Side-effects can be divided into short term (acute) side-effects that happen during or soon after your treatment, and long term side-effects occurring months or years later.
Some side-effects are common, whilst others are rare. As your treatment progresses you may experience some side-effects.
Not everyone will experience all of these reactions. If you do experience any of the following side-effects, do not worry, they are normal reactions to treatment. They usually begin about half way through the course of treatment, may last for several weeks after it has finished and then slowly settle down. Please tell us how you are feeling, particularly if your symptoms worsen, so that we can advise you.
Headache
If you develop frequent headaches during your treatment that are not relieved by pain killers, it is important that you are given the correct medical advice and medication. Please inform your nurse, radiographer or doctor immediately.
Tiredness (fatigue)
Radiotherapy can make you feel more tired than usual, especially if you have to travel a long way for treatment each day. Fatigue is most common in the first few months after treatment, but has usually improved significantly by six months. Only rarely does it last longer than this.
There are some things you can do to help yourself
- Gentle exercise can help reduce the symptoms of fatigue.
- Having enough to drink can prevent tiredness from dehydration.
- Small meals or snacks eaten more often than three times a day may be easier to face.
- Try to get a good night’s sleep where possible, a daytime nap may help.
- Try to ‘pace’ yourself, listen to what your body is telling you, rest if you need to.
- Pick out the things you enjoy, and try to accept help with other tasks.
- Little and often is the rule of thumb.
There is a Macmillan information leaflet about fatigue available. If you would like a copy, or support with your fatigue please ask a member of staff.
Somnolence Syndrome
Somnolence syndrome is a delayed side-effect of radiotherapy which occurs several weeks after treatment has finished. This is severe fatigue and exhaustion as described above. Please be aware that this can last for several weeks.
This is a normal and expected reaction to radiotherapy. Please contact your Clinical Nurse Team if you have any questions or concerns.
Skin reaction
Before you go in for your treatment the radiographer will explain what will happen to your skin and how to look after it. They will also give you a leaflet to take home.
The skin in the treated area may start to redden or darken around 10 days after starting your radiotherapy. It may become dry and itchy. Avoid hair removal where possible, including shaving, unless advised otherwise by your consultant, nurse or radiographer.
Hair loss
The hair follicles (roots) are very sensitive to radiation. Any hair directly in the treatment field, will gradually fall out during the course of treatment or shortly afterwards. You may start to notice your hair thinning 2-3 weeks after starting your radiotherapy. This hair loss is usually temporary.
When the course is finished your hair will slowly start to grow back but, in places, it may not be as thick as before. The texture and colour of the new hair may have changed. It can take up to six months before your hair re-grows. Sometimes there are areas of the scalp where the hair may not grow back at all.
A wig can be provided for you if you would like one. Please ask your nurse, radiographer or doctor. Turbans, scarves or hats are attractive alternatives to a wig. You may find wearing a hair piece, cap or hat more comfortable. Any head wear worn should not be too tight. There is a hair loss workshop and support available for anyone experiencing hair loss. For more information please contact the Sir Robert Ogden Macmillan Centre.
Macmillan Cancer Support has a booklet about coping with hair loss, which they will send to you free of charge. Alternatively, you can collect a copy from one of the information lounges.
Nausea and vomiting
It is rare to experience either of these side-effects while you are having treatment – but if you do have any problems please inform your nurse, radiographer or doctor.
Anti-sickness medication can be prescribed if necessary.
Taste changes
Occasionally, people may notice that their sense of taste alters during their radiotherapy and illness. Usually this is temporary, and it will gradually return to normal after the radiotherapy is finished.
Some people experience a sore mouth or throat depending on the area being treated. If you have any problems please speak to your radiographer or the nurses in Princess Royal Suite.
Hearing
If radiotherapy is delivered close to an ear, then it is sometimes possible for inflammation inside to temporarily cause some hearing loss on that side. This can sometimes last for a few weeks or months
Anxiety and emotional stress
During treatment many people feel stressed, anxious, depressed or at times unable to cope. If you or your family feel that they need someone to talk to we are able to offer appropriate help and advice. Please discuss any problems with your nurse, radiographer or doctor.
Long term effects
There are some side-effects that can develop many months or years after the radiotherapy. They depend on which part of the brain has been treated and the dose given. If for instance the pituitary gland (a part of the brain that produces hormones) receives a certain dose, regulation of some of the hormones can be upset. This can be treated by hormone replacements. Your doctor will tell you if you are at risk of pituitary under-activity or other problems.
Patients who live many years after radiotherapy may experience some cognitive effects (e.g. memory disturbance). Usually these are subtle and do not interfere significantly with day-to-day life. Similarly, there is also a very slightly increased risk of developing other brain tumours in the future.
Great care is taken to ensure radiotherapy does not affect your vision. However some patients may be at a slightly higher risk of cataracts many years after treatment. There may also be situations where a tumour lies close to an ear where there will be a risk of hearing loss in the long-term. Modern radiotherapy seeks to minimise these risks by limiting the doses delivered to normal brain tissue. However, these risks are always considered carefully by your doctor before offering radiotherapy. Your oncology team will discuss any predictable long term side-effects with you.
Steroid treatments
When giving radiotherapy to the brain it is often necessary to use a steroid drug (such as Dexamethasone). The purpose of the steroid is to reduce the amount of swelling (oedema)around the treatment area. An information leaflet is available, please ask a member of staff.
After treatment has finished
Some people find their symptoms temporarily get worse after radiotherapy has finished. This may make you think that your tumour is growing back. However it may simply be a reaction to the radiotherapy. If you find your symptoms get worse please discuss it with your nurse or doctor. You may need to increase or re-start your steroid treatment.
Your doctor will usually see you in the outpatient clinic approximately 4-6 weeks following your treatment.
Then your doctor will arrange to see you as necessary. Please discuss any problems and worries you may have with them at these appointments.
If you are worried about anything to do with this illness or treatment between your appointment visits, please contact your Key Worker or GP.
Further information and support
If you have any questions please ask your hospital team. We all have our own ways of coping with difficulties. Some people have a close network of family and friends who provide emotional support. Others would rather seek help from people who are not involved with their illness. The following are also available as sources of information and support that you may wish to use.
Clinical Nurse Specialists (CNS)
Your CNS is available to discuss any aspect of your treatment with you. You will be seen by a CNS before and during your treatment. This is to offer support and advice about the practicalities and effects of your treatment and answer any questions you may want to ask.
Your CNS will also assess and discuss any physical, psychological, social, occupational and spiritual needs that you may have. They can refer you to other services if needed, for instance, benefits advice. You should be given a ‘key worker’ as a contact for support through your treatment; this is usually your CNS.
Macmillan Specialist Radiographer and Macmillan Radiotherapy Nurse Specialist
Sometimes people need more help if they are feeling depressed, very anxious or are having problems with their Radiotherapy. If this is the case you may benefit from seeing the Macmillan radiographer or nurse specialist.
Your oncologist, radiographer or nurse can refer you at any point before or during your treatment.
Refreshments
There is a restaurant and coffee shop available on Level 0, which are open daily. They serve drinks, light snacks and hot meals. Vending machines are also available in the main radiotherapy waiting room and Level 0. There is also a shop on Level 0 with books, papers and snacks.
Hotel Bexley Wing
Patients having radiotherapy or chemotherapy sometimes use the hotel if they have a long way to travel. The hotel is located on the 8th floor of Bexley Wing and offers 19 twin rooms and 1 single room. All have en-suite, tea and coffee making facilities, a mini fridge, towels, hairdryer and digital television. There are two rooms with wheel chair access and a wet room. Patients are able to stay free of charge. There is a charge for relatives if they are staying in their own room.
Meals can be purchased (at breakfast and lunch) if you are able to make your way to the restaurant in the Bexley atrium. At other times you will need to have something you have brought from home or purchased. There is a very small fridge for your personal use. There are no staff after 4pm until the next morning in this facility.
For further details please contact the Hotel Co-ordinator.
Out of hours please contact the Non-Surgical Oncology Nurse Practitioner through main switch board.
Local Support Services
Leeds Cancer Support
Leeds Cancer Support complements care provided by your clinical team. We offer access to information and a wide range of support, in a welcoming environment for you, your family and friends. We can be found in the information lounges in Bexley Wing and also in the purpose built Sir Robert Ogden Macmillan Centre on the St James’s Hospital site.
The Sir Robert Ogden Macmillan Centre
This centre offers a variety of free health & wellbeing and supportive therapies for patients, their family members and carers. These include hypnotherapy, mindfulness coaching, acupuncture (for hot flushes) and pilates.
Contact numbers for Leeds Cancer Support
Maggie’s Centre
If you or someone you love has cancer you may have lots of questions. Maggie’s is a warm, welcoming place where you can meet people who are experiencing similar things to you.
You may also be able to find support groups specific to your needs and get advice and information from their professional staff. You don’t need an appointment and all support is free.
National Support Organisations
Car Parking
When you are coming for radiotherapy planning and treatment your parking is free in the on-site multi-storey car park.
Please ask for more information at the radiotherapy main reception desk.
How to find us

St James’s University Hospital – site plan