Most cancers of the rectum are treated by surgery. However, in some cases we recommend a course of radiotherapy before your operation or as the main treatment for your rectal cancer. The choice is made after considering a number of factors including the size and position of the tumour.
This leaflet supports the information you will receive from your Clinical Oncologist (who is a specialist doctor in cancer treatment). His/her team will be caring for you during your treatment. This team will include radiographers and clinical nurse specialists but may also include social workers, physiotherapists, occupational therapists and dietitians.
This leaflet also explains the side-effects that you may experience during and after treatment. These effects vary from one person to another, so the information is given as a general guide.
The healthcare team looking after you will explain your treatment and the side-effects in detail. If you have any questions after reading this leaflet, please speak to the team looking after you or ring the numbers at the end of leaflet. Staff will make every effort to meet your individual needs or will direct you to the person who can help.
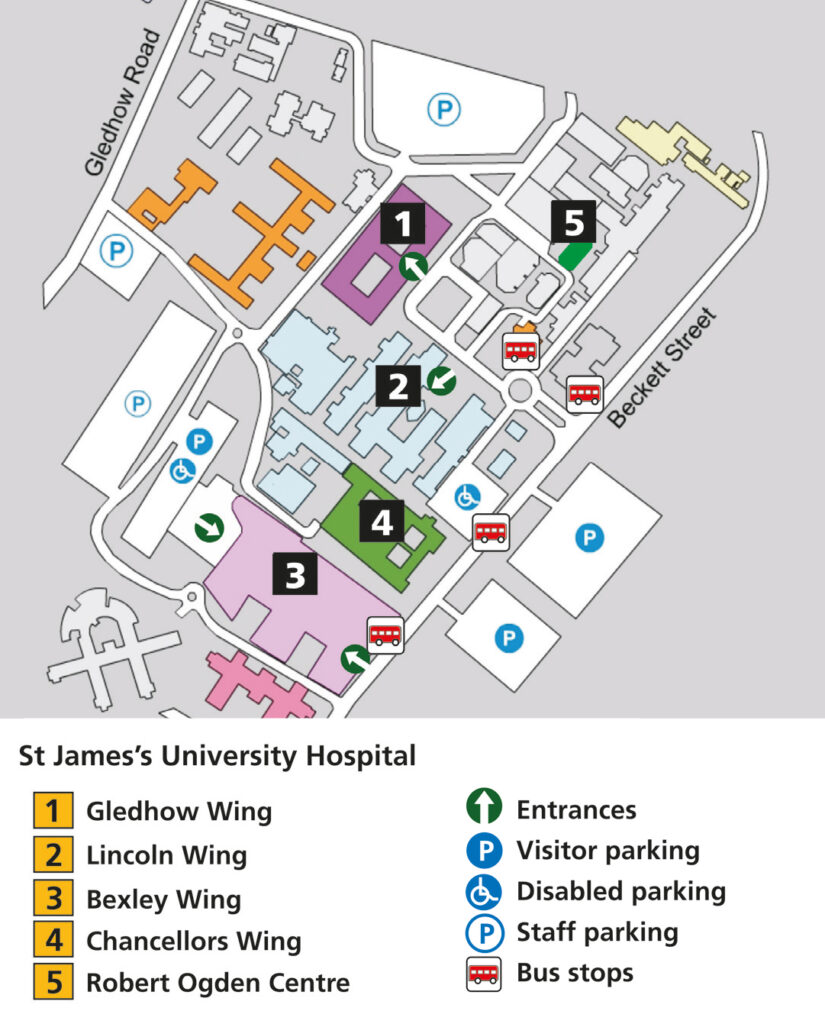
All your radiotherapy planning and treatment will take place in the Radiotherapy Department on Level -2, Bexley Wing, Leeds Cancer Centre, St James’s Hospital, Leeds (LS9 7TF).
Please do not bring any valuables into hospital with you as the Trust cannot accept liability for loss or theft.
What is radiotherapy?
Radiotherapy is the use of high energy X-rays and other types of radiation, to treat cancer. The radiotherapy causes damage to the cancer cells in the treated area. Although normal cells are also affected, they can repair themselves and are able to recover.
Radiotherapy is a local treatment. This means it only affects the part of the body that is treated. You do not feel anything during radiotherapy and you will not be radioactive.
You may hear a buzzing noise when the machine is switched on.
It is perfectly safe for you to be around others, including children and anyone who may be pregnant, throughout your treatment.
You will have your radiotherapy on a treatment machine called a Linear Accelerator as shown in the photograph. You will see your radiographers at each treatment session, and they will be happy to answer any questions you may have.

How often is it given?
Our usual treatment involves five days of radiotherapy, given daily Monday to Friday. However, your treatment may not start on a Monday.
You may need to be treated on a weekend due to a bank holiday and we will let you know if this is the case. Your radiographer will be able to explain the details of your individual radiotherapy appointments.
Your treatment will usually be given as an outpatient.
Important advice before your treatment
Pregnancy
It is very important that patients of childbearing potential are not pregnant at the start of a course of radiotherapy and that they do not become pregnant during a course of radiotherapy because it can have an effect on the unborn child. Use an effective form of contraception, for example condoms, coil, depo injection or contraceptive pill.
For more information see the ‘Contraception and pregnancy during cancer treatment’ leaflet. Please do not hesitate to ask your doctor or nurse if you have any questions or concerns about these issues.
Who will I meet?
Therapeutic radiographers
Radiotherapy is given by therapeutic radiographers of any gender, who are highly trained in the accurate planning and delivery of radiotherapy treatment.
You will see your radiographers at each treatment session and they will be happy to answer any questions you may have.
Student radiographers
The radiotherapy department is a training centre for therapeutic radiographers. They are supervised at all times. If you do not wish students to be present, please speak to a member of staff. This will not affect your treatment or care.
Others involved in your care
You may meet other staff whilst you are coming for radiotherapy. Everyone you meet will introduce themselves, tell you their job title and explain the role they have in your care.
Visiting us before your treatment
If you would like to visit the radiotherapy department before starting treatment, please call 0113 206 7603. This visit can be very useful as you can find out more information about radiotherapy and ask questions.
Planning your treatment
Your first appointment for radiotherapy will be a planning appointment. This will be used to gather all the information we need to accurately plan your treatment. We will contact you by phone, with an appointment for your radiotherapy planning session. Directions to the hospital and transport arrangements will be discussed with you at this point.
Some tests and scans may be needed to help plan your treatment. We will explain which of these you will need when your appointment is made. You may see your clinical oncologist (or a member of their team) at this appointment. This is an ideal opportunity for you to ask questions. If you have not previously consented to your treatment you will be asked to sign a consent form.
This appointment may include:
- Signing a consent form that says you agree to have treatment, (if it has not been done already);
- a nursing assessment; and
- a planning CT scan.
What to bring with you:
- a list of all questions you may have;
- an up-to-date list of all the medications you are taking;
- any medication that you may need during your visit;
- something to eat and drink and something to occupy yourself with, as this first visit can be quite lengthy (up to two hours).
- When attending the hospital always bring spare stoma equipment with you if you have been fitted with a stoma bag.
Radiotherapy planning scan
In order to plan your treatment, you will have a planning CT scan. This is done on a machine called a CT Scanner, shown here in the photograph. It allows the images from the scan to be sent to the radiotherapy computer planning system.
There will be several members of staff present at your scan. These will include therapeutic radiographers, and possibly a mould room technician and a dosimetrist (the person who will produce the computer plan for your treatment).

Planning scans are not diagnostic examinations and will not be reported on as such.
The scan appointment usually takes 10-15 minutes. Your bladder will need to be comfortably full for the scan, although you do not need to arrive with a full bladder. The radiographers will explain how to prepare your bladder. You will be asked to undress from the waist down and will be given a gown to wear. You will be lying in the position shown in the photograph.

It is important that you are comfortable as you will have to lie in this exact same position for your treatment each day. Please tell the radiographers if you are uncomfortable.
The radiographers will draw some marks on you, to be used as a reference for your treatment.
You will then be scanned, which will only
take a few minutes and at the end of the scan the skin mark will be replaced by a small permanent mark (tattoo).
These permanent marks help us to ensure that you are in the same position each day. It also means that you can wash without worrying about your marks coming off.

You may also need an MRI scan, again for planning purposes. This involves a separate appointment in our department. This could take place the same day as the CT scan, or may be on a different day. Your radiotherapy is individually planned by your oncologist and a specialist physics team using information from the CT and MRI scans.
Contrast (dye)
A special contrast agent, often called a dye, may be used for your scan to make specific organs, blood vessels and/or tissue types ‘stand out’. This can make it easier for the oncologist to plan your treatment. This contrast is only needed for the planning scan, not each treatment.
If used, the dye is given through a very small plastic tube called a ‘cannula’ into a vein in your arm. You should tell the radiographer if you have any allergies, but they will go over this with you before they use any dye. The radiographers will advise you about drinking plenty of fluid after your injection.
Contrast side-effects
You may notice a warm feeling throughout your body and have a metallic taste in your mouth. You may also feel as if you have passed urine. This will pass very quickly. There is a slight risk of an allergic reaction to the injection, such as skin rash, but this very rarely may lead to other complications.
The staff in the radiotherapy department are highly trained to manage any complications and again the risk is very small.
You will be able to drive and go to work after your scan.
Following the scan the radiographers will give you the time of your first appointment on the treatment machine, which is most likely to be a couple of weeks after the planning visit. The radiographers will talk to you about any further appointments you have.
Having your radiotherapy
When you arrive for your treatment you should go to the radiotherapy main reception desk at the entrance of the radiotherapy department. On the first occasion you will be given all your appointments. This includes an appointment to see our nurses on the first day. You will also be escorted to the waiting area for your machine. The radiographers will explain what will happen and answer any questions that you may have.
Treatment is usually given daily, Monday to Friday, however your treatment may start on any day of the week. Whenever possible you will be treated at the time of day that suits you, but this cannot always be arranged or guaranteed. There may be occasions when you may have a longer stay in the department or be asked to attend at a different time, for example to see your oncologist.
You will need to prepare your bladder each day before treatment by drinking a certain amount of fluids before your treatment time. Again, this will be explained to you.
You may need to undress and put on a gown; the radiographers discuss this with you when you first attend the department. The radiographers will position you, and adjust the treatment couch and machine to the correct positions.
For the first few treatments and also intermittently during treatment we will also take images to check the accuracy of the treatment which will take a few more minutes.
These images do not monitor your condition but are purely for treatment accuracy.
You will be asked to stay as still as possible during the treatment but you should breathe and swallow normally. Once you are in the correct position the radiographers will leave the room to switch on the machine. You will only be alone for a few moments at a time. The radiographers will be watching you on a closed-circuit TV (CCTV) monitor during treatment.
The CCTV camera is not recording or saving any images. There is also an intercom system so the radiographers can talk to you. If you would like to listen to music during your treatment, please let us know.
It is very important that you do not miss treatment days as it may make your treatment less effective. If you feel you are unable to attend for any reason please telephone us so that we can discuss this with you. If you have any queries about your appointment times please discuss these with the radiotherapy coordinators on your treatment unit.
On some days the radiotherapy department may be busy and there may be a delay before your treatment. We will keep you informed of any delays. Please see the delay signs in the waiting areas.
It may be a good idea to bring something to eat and drink with you, including any supplement drinks you have been asked to have and any medication you may need. Bexley Wing also has a variety of places where food and drink can be bought during the day.
Side-effects
Side-effects can be divided into short term (acute) effects which happen during or soon after treatment, and long term side effects occurring months or years later.
Some side-effects are common, whilst others are rare. The area and amount of treatment given to you will affect which side effects are most likely to happen to you. Your oncologist will discuss this with you.
Our Review Clinic nurses will also do a follow-up telephone call with you 10 days after you have finished your radiotherapy. They will discuss any symptoms you may be experiencing, and also explain any medication you may need.
If you develop any radiotherapy side effects you will be given advice and support by your healthcare team. Below is a list of side effects along with how likely it is for that particular side effect to occur.
Here are some definitions to help you:
- Common – More than 10 in every 100 (more than 10%) people will develop this side-effect.
- Occasional – Between one and 10 in every 100 (1 to 10%) people will develop this side-effect.
- Rare – Less than one in 100 (less than 1%) people will develop this side-effect.
However, please be aware that each patient can react differently to treatment. You may experience side effects at different times and to varying degrees, compared to other patients having the same treatment.
Short term side-effects
Most side-effects are common and are temporary.
Radiotherapy side-effects
Tiredness (fatigue)
Common
Nearly all patients having radiotherapy will feel tired. Be prepared to take things easy during treatment and allow for extra rests. There is a Macmillan information leaflet on Fatigue available and if you would like a copy, or support with your tiredness please ask a member of staff.
Fatigue usually improves in the weeks to months after treatment. Try to continue with some of your normal routines and activities if possible. If you are struggling with tiredness you should let your key worker / clinical nurse specialist know.
Rare
Whilst some tiredness is common it is rare for you to stop being able to do day-to-day tasks.
Things you can do to help with tiredness include:
- Gentle exercise can help reduce the symptoms of fatigue.
- Having enough to drink can prevent tiredness from dehydration.
- Small meals or snacks eaten more often than three times a day may be easier to face.
- Try to get a good night’s sleep where possible, a daytime nap may help.
- Try to ‘pace’ yourself, listen to what your body is telling you, rest if you need to.
- Pick out the things that you enjoy, and try to pass on other tasks.
- Little and often is the rule of thumb.
Bowel problems
Radiotherapy includes treating some of your normal bowel as well as the cancer and can cause inflammation, swelling and soreness of the lining of the bowel. These side-effects usually start in the week after you finish your treatment but usually settle after a few weeks.
Common
- Diarrhoea (i.e. more liquid poo, that is passed more often). If you have a stoma you may need to change or empty your bag more often;
- Needing to get to the toilet quickly (urgency);
- Bleeding or mucus loss from the back passage.
Occasional
- Abdominal (tummy) bloating and discomfort;
- Feeling of fullness in the back passage or pain (particularly if your tumour is low down).
Things you can do to help with bowel side-effects include:
- If you need to open your bowels (have a poo) four or more times more than is usual for you in a day, then tell the radiographers, your doctor or nurse. If this starts after you have finished treatment tell your specialist nurse or ring the radiotherapy department for advice.
- You will be given anti-diarrhoeal tablets to take, called “loperamide”. If you get diarrhoea you should start taking these as instructed.
- If you have a stoma please make sure you bring spare stoma equipment with you each day.
- If you have pain or discomfort in the back passage, pain killers can help. These can be tablets, such as Paracetamol or gels/creams that can be applied to the skin around the back passage (such as instillagel).
- Some people feel more confident if they wear a pad in case of leakage.
Skin reaction
Common
The skin in the treated area (around your back passage or buttocks) starts to redden or darken about 10 days after the start of radiotherapy treatment. It may become dry and itchy. Sometimes, later, it may peel and become weepy.
After any redness or darker skin patches fade, a few people may have pigmentation (brown or darker coloration) left on the skin and these areas will also be more sensitive to sunlight than before.
Things you can do to help with skin reaction include:
- Before you go in for your treatment the radiographer will explain what could happen to your skin and how to look after it. They will also give you a leaflet to take home. If you are concerned about your skin reaction please talk to your radiographers or contact the review clinic nursing staff in the Princess Royal Suite, telephone: 0113 206 7587.
- You should be given barrier cream before you start treatment. Please use twice a day as instructed by the radiographers or nurses. Please ask the team if you don’t receive this.
- The team will recommend different creams or dressings if you need them. Do not use your own creams in the radiotherapy treatment area as they can make your skin reaction worse.
- Avoid hair removal where possible, including shaving, waxing, cream and lasers unless advised otherwise by your consultant, nurse or radiographer.
Other side-effects from the radiotherapy are less common
Bladder problems
Your bladder will also be included in the treatment area (as it is very close to the back passage), causing these side-effects:
Occasional
- Pain/stinging on passing urine (when you’re having a wee);
- Passing urine more often;
- Needing to get to the toilet quickly (urgency).
Things you can do to help with bladder side effects include:
- Avoid drinks that could irritate the bladder such as tea, coffee, alcohol and most concentrated fruit juices. Decaffeinated tea and coffee is fine to drink. Drinking cranberry juice may help with an irritated bladder. However please note that cranberry juice may interfere or cause problems with some medication (for example Warfarin). Therefore, please check with your hospital team first.
- If it stings when you pass urine, tell the radiographers, your doctor or nurse. You may have a urine infection and so your team will ask you to provide a urine sample.
- Some people feel more confident if they wear a pad in case of leakage.
Pubic Hair loss
Occasional
Only hair in the treated area will stop growing and may fall out. Sometimes hair will not grow back after treatment.
Back pain
Occasional
You may notice some pain in your lower back or buttocks. Sometimes the pain can travel down the back of the legs. If this happens please tell your radiographer as soon as possible.
Usually this pain is mild and needs no treatment. On rare occasions you may need pain killers, and/or a slight modification of your radiotherapy (this will be discussed with you and should not affect how well your treatment works).
Nausea and vomiting
Occasional
If you have any nausea or vomiting this can be controlled with anti-sickness medication, which you will be given to take home. Only a small number of patients experience this.
Long term side-effects
The long term side-effects depend upon the specific treatments you have. They are due to a combination of the radiotherapy and the type of surgery needed (if you require an operation).
Surgery
Your surgeon will advise you on the most appropriate surgery for you. The type of surgery you have will determine the long term side effects you may experience.
Your surgical team will discuss these with you. Many people will have a stoma, which can be permanent or temporary (to allow the bowel to heal).
Long term side-effects from surgery include:
- changes in your bowel habit, once the temporary stoma has been reversed,
- changes in how your bladder works and,
- if you have a penis: impotency or erectile dysfunction (being unable to attain and maintain an erection).
Long term side-effects of pelvic radiotherapy
Radiotherapy can cause some scarring changes to the normal healthy tissues around the tumour treated with radiotherapy. This can lead to long term side-effects months and years after treatment. There are investigations and treatments we can recommend to help support you if you develop any of these problems.
Bowel problems
If you undergo surgery where the bowel is joined up again, there is an increased risk of opening your bowels (having a poo) more often each day. If you have a permanent stoma then it may be more active than if you had not had radiotherapy.
Common
- Permanent change in bowel habit – having your bowels open more often in a 24 hour period.
- Urgency to get to the toilet or a need to open your bowels as soon as you feel the desire.
Occasional
- Occasionally urgency to open your bowels can be associated with not being able to control it, called ‘faecal incontinence’. This may cause soiling of clothing or leakage.
- Long term pain or discomfort in the back passage.
Things you can do to help with bowel side-effects include:
Review your food and drink habits: After radiotherapy you may find that you pass wind more often and have less control of when this happens. There can be many reasons for this:
- eating too many vegetables (see below);
- food containing starch and dietary fibre;
- some medication used to regulate bowel habits.
Foods that may cause wind include:
- pulses (such as peas, beans and lentils);
- vegetables from the brassica family (such as brussels sprouts, cabbage and artichokes);
- onions;
- high-fibre food such as bran;
- fizzy drinks.
If you are finding you have excess wind, urgency or diarrhoea then please ask your clinical nurse specialist for advice.
Bladder problems
Common
Needing to pass urine more often, including passing urine at night.
Occasional
Not being able to control your bladder as well – causing dribbling and leakage.
If you are finding any urinary symptoms a problem please ask your clinical nurse specialist for advice.
Other things that may help you with bladder and bowel side effects:
- Macmillan toilet card
If you want to go to the toilet more often, or feel that you can’t wait when you do want to go, you can get a card to show staff in shops, pubs and other places. The card allows you to use their toilets without you being asked awkward questions. You can get the cards from your radiographer or the information lounge in the radiotherapy department. - Pelvic Floor Exercises
You may have a more urgent need to use the toilet and difficulty in holding your bladder or bowels. This is because radiotherapy affects the muscles in your pelvic floor which are used when controlling your urges to pass water or stools. Doing pelvic floor exercises 3-4 times per day will help to strengthen these muscles and improve these side-effects.
Please ask your nurse specialist for more information.
Sexual function
Intercourse (sex) is safe during treatment. However you must abstain from receiving anal sex throughout treatment and for another two months afterwards.
Sexual problems in patients with female reproductive organs
Common
Menopause and Infertility
Radiotherapy should not be given in pregnancy because of the potential harmful effects on the baby. If you have the potential to become pregnant, you MUST use contraception during treatment, and also for one year after your treatment has finished.
If you have not gone through the menopause, this treatment can bring forward your menopause and cause infertility so you will no longer be able to have children. You may notice your periods becoming irregular during or after treatment. If you have not completed your family, please discuss this with the doctor before starting treatment.
We can refer you to a specialist to discuss the storage (freezing) of eggs or embryos, which could potentially be used in future.
The symptoms of early menopause can include:
- hot flushes and sweats
- vaginal dryness
- passing urine more often
- lower interest in sex
- tiredness and difficulty sleeping
- dry skin
- aches and pains
- mood swings, poor concentration, lower confidence and changes in memory.
Irregular periods
You may also notice your periods becoming irregular during or after treatment. However, as mentioned before, if you are of childbearing potential you should continue to use contraception during your treatment and for one year after your treatment has finished. Since radiotherapy may harm an unborn child it is very important to avoid pregnancy during treatment.
Vaginal dryness and tightness
Some people may also experience vaginal dryness and pain during intercourse. Your vagina may also become narrower following treatment. These side-effects can be reduced by using a vaginal dilator (which we will give you), lubricating jelly or resuming sexual intercourse.
A member of the team will discuss this with you and give you the dilators and our information leaflet ‘Vaginal Care after Radiotherapy’. Advice on hormone replacement therapy is also available.
Low sex drive
Fatigue and anxiety associated with treatment can affect sex drive. This may only recover slowly after treatment.
Things you can do to help with these sexual side-effects include:
- If you are finding any sexual side effects a problem please ask your clinical nurse specialist for advice.
- With your hospital team and your GP you can consider hormone replacement therapy to improve menopausal and vaginal symptoms and low sex drive.
- For vaginal symptoms, regular vaginal dilator use with lubricating jelly is a good place to start and you will be given advice on this.
Sexual problems in patients with male reproductive organs
Common
Infertility
Radiotherapy can affect the quantity and quality of sperm production. This can lead to increased rates of abnormality in children that are conceived during or after treatment.
You are advised to use contraception for one year after treatment.
If you would like to have children in the future, you should discuss this with your doctor before starting radiotherapy so we can arrange storage (freezing) of some sperm. This can then be used at a later time if needed.
Erectile problems and changes in ejaculation
There is an increased risk of erectile dysfunction (being unable to attain and maintain an erection) if you have received radiotherapy.
If this is a problem, then you should discuss it with your GP or hospital team. They may recommend a medication treatment or you may be referred to a specialist clinic. Your ejaculation experience may also change, including dry (no fluid) or painful ejaculation.
Low sex drive
Fatigue and anxiety associated with treatment can affect sex drive. This may only recover slowly after treatment.
Things you can do to help with these sexual side-effects include:
- If you are finding any sexual side effects a problem please ask your clinical nurse specialist for advice.
- With your hospital team and your GP you can consider the use of medications to help with erectile problems (such as Viagra) and further investigation of your symptoms.
Skin
Common
If you undergo complete removal of your back passage and anus after radiotherapy, the bottom wound may be slow to heal. This can also be a problem even if you do not have radiotherapy.
Your skin may become dry and less supple, and sometimes you can develop darker skin and small broken veins. Treated skin will be more sensitive to sunlight.
The radiographers will advise you at the end of your treatment, but using barrier creams can help.
Cancers caused by the radiotherapy
Rare
When you have had radiotherapy there is a risk that a new cancer can develop many years later caused by the treatment. However, this is rare. Accurate information on this is not available and the benefits of the treatment far outweigh any potential risk in the future. If you are at all concerned then please speak to your medical team.
Bone health (Pelvic insufficiency fractures)
Occasional
There is an increased risk of fractures of the bones in the pelvis after radiotherapy. These are usually “hairline” and treated with painkillers.
If you have any new bone pains, please discuss these with your GP and hospital team.
Nutrition
It is important that you are well nourished and drink plenty of fluids during your treatment in order to keep you healthy and to help your body to heal. What you eat will affect your bowel habits so ask for advice.
How well you can eat and drink varies, depending upon where the cancer is and on the details of your treatment.
If needed, we will refer you to one of our specialist dietitians.
After your radiotherapy
Most people will have an operation at around 8-14 weeks after finishing radiotherapy. This is to give time for the tumour to shrink down. Before an operation you will have scans (usually a CT and MRI scan). These scans will be arranged by your local hospital and your team will advise you when they will happen. This is usually between 6-10 weeks after finishing your radiotherapy. The scans will be discussed at your local cancer meeting (MDT) and a plan made for your operation date.
Some patients will have a ‘complete response’ where their tumour completely disappears after radiotherapy. This happens in around 15% of patients (3 in every 20 people treated). In patients who have smaller tumours, avoiding surgery may be the goal of treatment and so this number is much higher. If your tumour completely disappears on the scans, you may be offered the opportunity to have ‘active surveillance’ (close monitoring) or a smaller operation. Your team will discuss this with you in more detail if you are in this position.
Research at Leeds Cancer Centre
Leeds Cancer Centre is a major centre for cancer research. You may be asked if you would like to help with some of the clinical studies. You are under no obligation to take part in any trials, and your treatment will not be affected in any way if you do not wish to take part. If you do take part in a clinical trial you may meet a research nurse or radiographer who will be helping to run the trial.
Further information and support
If you have any questions please ask your hospital team. We all have our own ways of coping with difficulties. Some people have a close network of family and friends who provide emotional support. Others would rather seek help from people who are not involved with their illness.
The following are also available as sources of information and support that you may wish to use:
Clinical Nurse Specialists (CNS)
Your CNS is available to discuss any aspect of your treatment with you. You will be seen by a CNS (this is normally your Colorectal Nurse) before your treatment. This is to offer support and advice about the practicalities and effects of your treatment and answer any questions you may want to ask.
Your CNS will also assess and discuss any physical, psychological, social, occupational and spiritual needs that you may have. They can refer you to other services if needed, for instance, benefits advice.
You should be given a ‘key worker’ as a contact for support through your treatment; this is usually your Colorectal Nurse.
Macmillan Specialist Radiographer and Macmillan Radiotherapy Nurse Specialist
Sometimes people need more help if they are feeling depressed, very anxious or are having problems with their treatment. If this is the case you may benefit from seeing the Macmillan radiographer or nurse specialist. Your oncologist, radiographer or nurse can refer you at any point before or during your treatment.
They currently cover topics such as:
- Pelvic Radiotherapy Late effects
- Managing bowel changes after treatment
- Pelvic floor exercises after treatment
- Side effects of treatment to the female pelvic area
- Side effects of treatment to the male pelvic area
- Coping with fatigue (tiredness)
Local Support Services
Leeds Cancer Support
Leeds Cancer Support complements care provided by your clinical team. We offer access to information and a wide range of support, in a welcoming environment for you, your family and friends.
We can be found in the information lounges in Bexley Wing and also in the purpose built Sir Robert Ogden Macmillan Centre.
The Sir Robert Ogden Macmillan Centre
This centre offers a variety of free health & wellbeing and supportive therapies for patients, their family members and carers. These include hypnotherapy, mindfulness coaching, acupuncture (for hot flushes) and pilates.
Contact numbers for Leeds Cancer Support
Maggie’s Centre
If you or someone you love has cancer you may have lots of questions. Maggie’s is a warm, welcoming place where you can meet people who are experiencing similar things to you.
You may also be able to find support groups specific to your needs and get advice and information from their professional staff. You don’t need an appointment and all support is free.
National Support Organisations
Hospital Contact Numbers
Most queries during treatment can be addressed to nursing staff or the radiographers. If required, they will contact the medical team on your behalf. However, during office hours, you may also wish to contact the ward where you have been treated or our chemoradiotherapy nurse specialist.
These numbers are provided below:
Car Parking
When you are coming for radiotherapy planning and treatment, your parking is free in the on-site multi-storey car park. Please ask for more information at the radiotherapy main reception desk.
Hotel Bexley Wing
Patients having radiotherapy or chemotherapy sometimes use the hotel if they have a long way to travel. The hotel is located on the 8th floor of Bexley Wing and offers 19 twin rooms and 1 single room. All have en-suite, tea and coffee making facilities, a mini fridge, towels, hairdryer and digital television. There are two rooms with wheel chair access and a wet room. Patients are able to stay free of charge. There is a charge for relatives if they are staying in their own room.
Meals can be purchased (at breakfast and lunch) if you are able to make your way to the restaurant in the Bexley atrium. At other times you will need to have something you have brought from home or purchased.
There is a very small fridge for your personal use. There are no staff after 4pm until the next morning in this facility.
How to find us
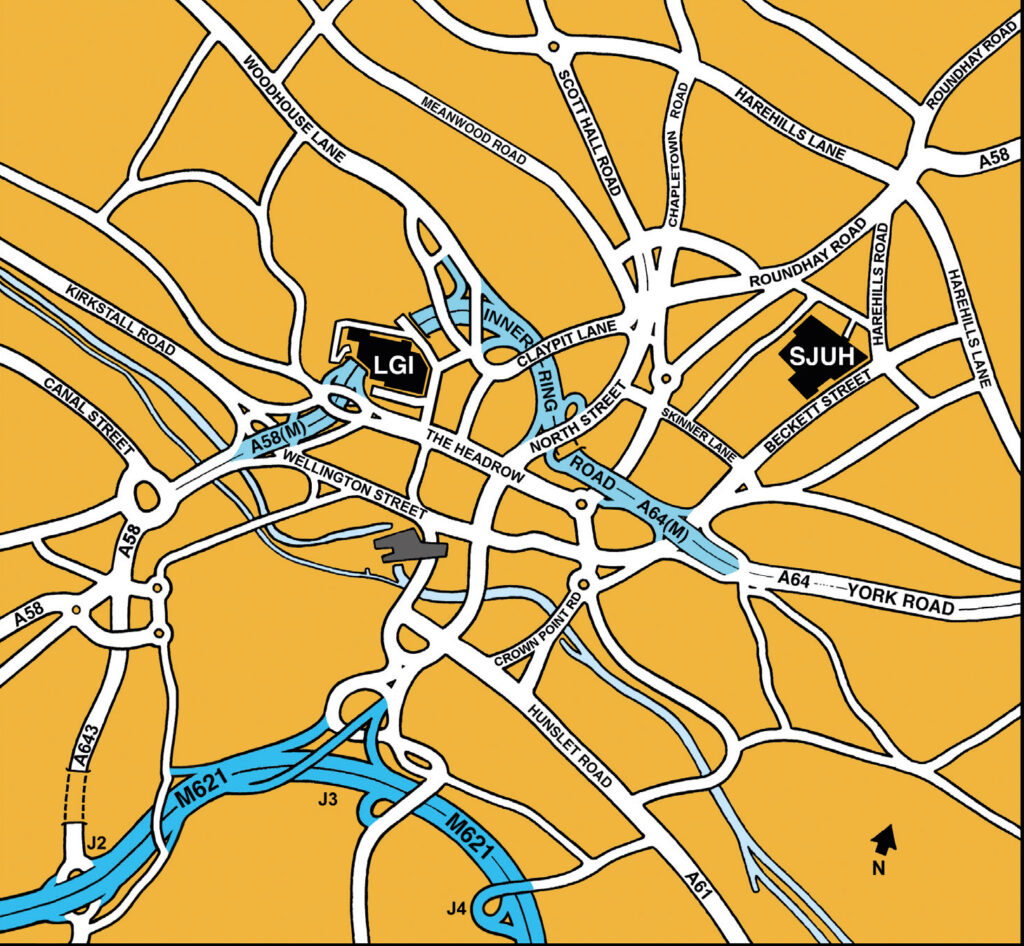
St James’s University Hospital – site plan