This leaflet aims to help you and your family understand more about your cancer treatment.
It will be given to you in addition to the information you will receive from your Clinical Oncologist (who is a specialist doctor in cancer treatment). Their team will be caring for you during your treatment. This team will include radiographers and clinical nurse specialists but may also include social workers, physiotherapists, occupational therapists and dieticians.
The leaflet describes radiotherapy planning and treatment. It also explains the side-effects which you may experience during and after treatment. Each person’s treatment will vary, so the information given is a general guide. The healthcare team looking after you will explain your treatment and the side- effects in detail.
If you have any questions after reading this leaflet, please speak to the team looking after you or ring the numbers at the end of the leaflet. Staff will make every effort to meet your individual needs or will direct you to the person who can help.
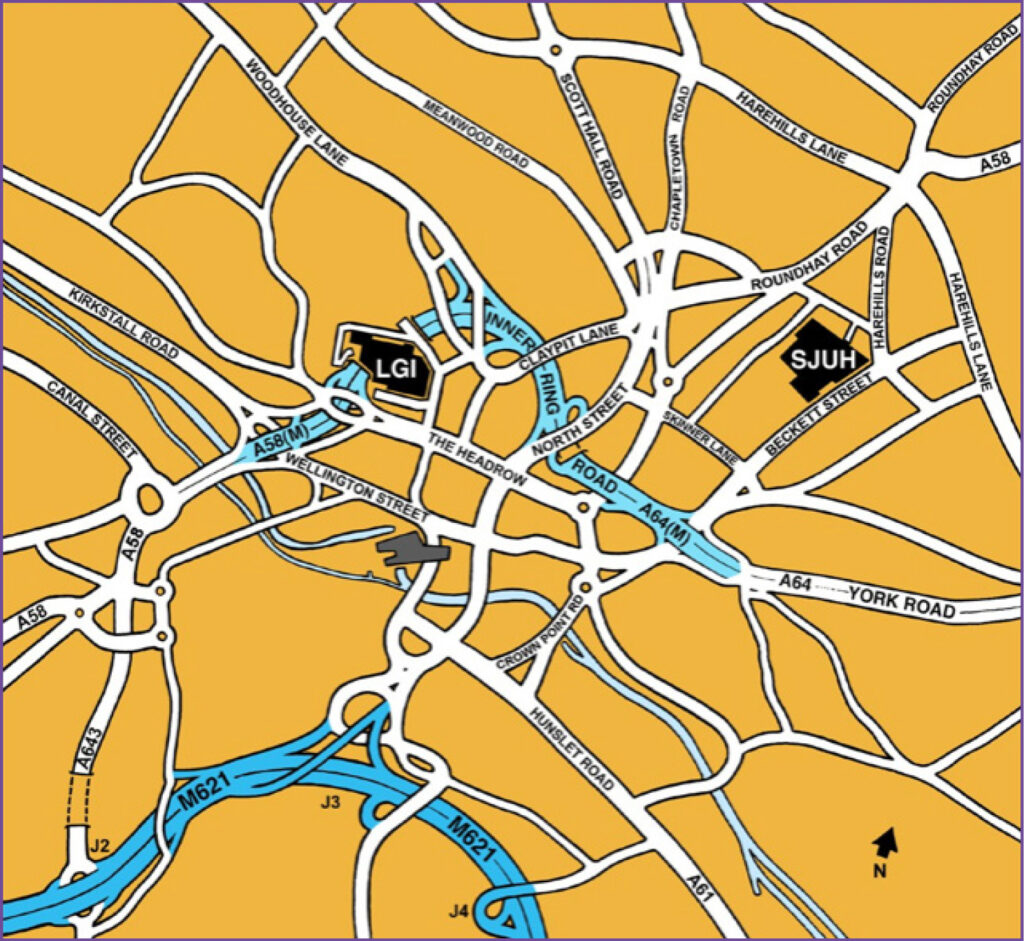
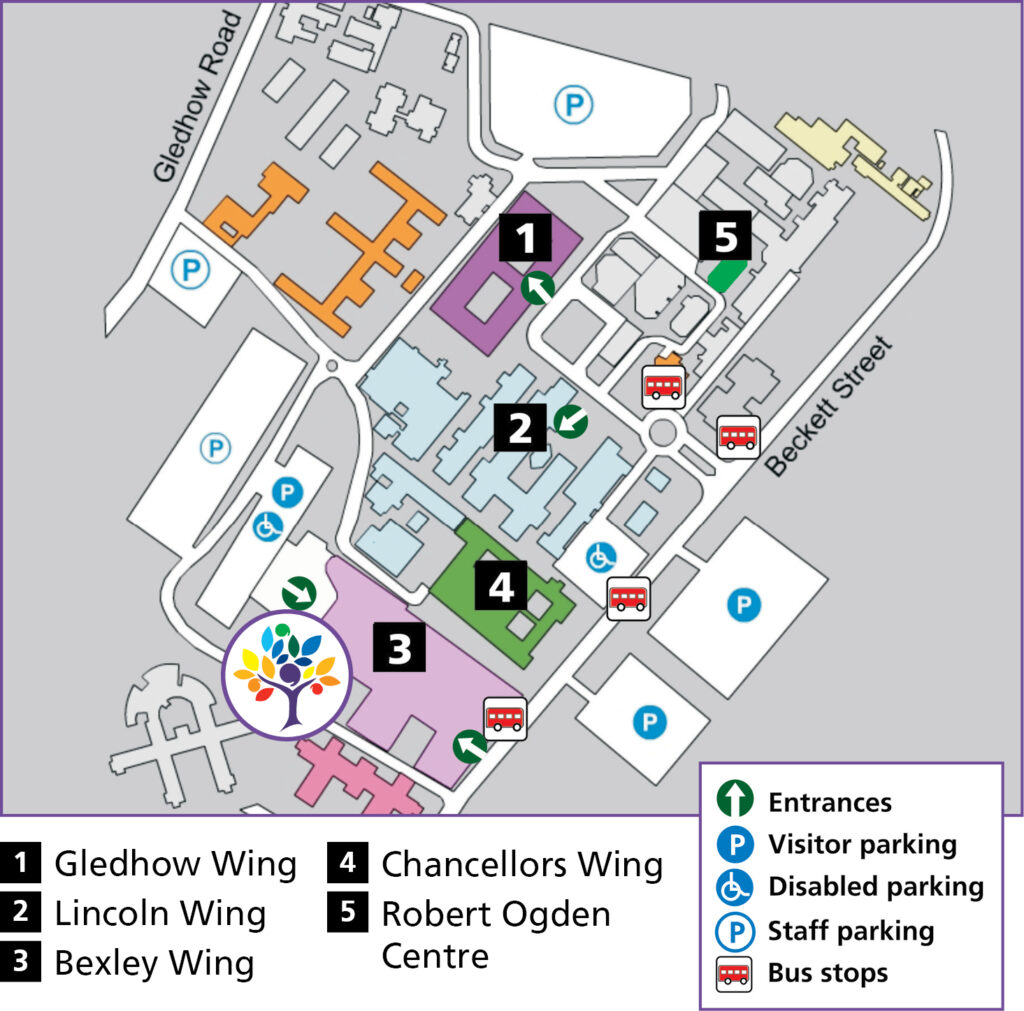
All your radiotherapy planning and treatment will take place in the Radiotherapy Department on Level -2, Bexley Wing, Leeds Cancer Centre (LS9 7TF).
Radiotherapy reception Tel: 0113 206 8940
Please do not bring any valuables into hospital with you as the Trust cannot accept liability for loss or theft.
Contacts
Radiotherapy Reception: 0113 206 8940
8.00am – 6.30pm Monday – Friday
(Radiotherapy related queries only)
Review Clinic/Princess Royal Suite: 0113 206 7587
8.30am – 6.00pm Monday – Friday
Transport: 0113 206 8726
Hospital switchboard: 0113 243 3144
Consultants
Dr Cooper’s Secretary: 0113 206 8234
Dr Cardale’s Secretary: 0113 206 7854
Dr Anderson’s Secretary: 0113 206 7822
Clinic Clerk (appointments): 0113 206 8346
Clinical Nurse Specialists
0113 206 7820 – this is an answer machine. Messages are picked up three times a day, and calls will be returned as soon as possible.
Emergency contact number
Tel: 0113 243 3144 and ask for the Oncology Patient Enquiries bleep holder. Contact this number if you feel seriously unwell.
What is radiotherapy?
Radiotherapy is the use of high energy X-rays and other types of radiation to treat cancer. The tissues of the body are made up of tiny building blocks called cells.
The radiotherapy causes damage to the cancer cells in the treated area. Although normal cells are also affected, they can repair themselves and are able to recover.
Radiotherapy is a local treatment.
This means it only affects the part of the body that is treated. When you are having your radiotherapy you do not feel anything and it does not make you radioactive. You may hear a buzzing noise when the machine is switched on. It is perfectly safe for you to be with other people, including children and pregnant people throughout your treatment. You will have your radiotherapy on a treatment machine called a linear accelerator as shown here in the photograph. You will see your radiographers at each treatment session and they will be happy to answer any questions you may have.

Treatment for each patient is planned individually, and even patients with the same type of cancer may not receive identical treatment. Radiotherapy may be used as your main treatment, or combined with other treatments such as surgery and chemotherapy.
How often is it given?
Radiotherapy is usually given over one day to seven weeks. This is a total of between 1-35 treatment days. Treatment is usually given daily, Monday to Friday however your treatment may not start on a Monday. There may be occasions when you may have a longer stay in the department or be asked to attend at a different time, for example to see your oncologist.
Radiotherapy is usually given over one day to seven weeks. This is a total of between 1-35 treatment days. Treatment is usually given daily, Monday to Friday however your treatment may not start on a Monday. There may be occasions when you may have a longer stay in the department or be asked to attend at a different time, for example to see your oncologist.
Your treatment will usually be given as an outpatient.
Visiting us before your treatment
If you would like to visit the radiotherapy department before starting treatment, please call 0113 206 7603. This visit can be very useful as you can find out more information about radiotherapy.
Who will I meet?
Therapeutic radiographers
Radiotherapy is given by therapeutic radiographers of any gender who are highly trained in the accurate planning and delivery of radiotherapy treatment. You will see your radiographers at each treatment session and they will be happy to answer any questions you may have.
Student radiographers
The radiotherapy department is a training centre for therapeutic radiographers. They are supervised at all times. If you do not wish students to be present, please speak to a member of staff. This will not affect your treatment or care.
Others involved in your care
You may meet other staff whilst you are coming for radiotherapy. Everyone you meet will introduce themselves, tell you their job title and explain the role that have in your care.
Pregnancy
It is very important that patients of child bearing potential are not pregnant at the start of a course of radiotherapy and that they do not become pregnant during a course of radiotherapy because it can have an effect on the unborn child. Use barrier contraception (i.e. condoms). In addition to this, use contraception during treatment and for six months afterwards.
For more information see the ‘Contraception and pregnancy during cancer treatment’ leaflet. Please do not hesitate to ask your doctor or nurse if you have any questions or concerns about these issues.
Planning your treatment
Your first appointment for radiotherapy will be a planning appointment. This will be used to gather all the information we need to accurately plan your treatment. We will contact you by phone, with an appointment for your radiotherapy planning session. Directions to the hospital and transport arrangements will be discussed with you at this point.
You may see your clinical oncologist (or a member of their team) at this appointment. This is an ideal opportunity for you to ask questions. If you have not previously consented to your treatment you will be asked to sign a consent form.
What to bring with you
- a list of all questions you may have;
- an up-to-date list of all the medications you are taking (including inhalers, sprays, vitamins or herbal products);
- any medication that you may need during your visit;
- something to eat and drink and something to occupy yourself with as this first visit can be quite lengthy (up to two hours).
Your planning scan
In order to plan your treatment you will have a planning CT scan. This is done on a machine called a CT Simulator, shown here. This is a CT scanner that allows the images to be sent to the radiotherapy computer planning system.

There will be several members of staff present at your scan.
Planning scans are not diagnostic examinations and will not be reported on.
Before your planning scan a radiographer will talk to you about bowel and bladder preparation. This usually involves the use of a ‘micro enema’. You will be given a leaflet to explain this.
It is important to have an empty back passage and a comfortably full bladder, both for your planning scan and during treatment. This is to ensure the accuracy of the treatment planning and delivery. If you struggle to keep your bladder full please tell the radiographer.
Important information about taking your Microenemas
Only use the micro-enemas on the days you are having radiotherapy. You do not need to use the micro-enemas on a weekend unless you are having a treatment session.
Please tell your radiographer if you are having frequent or loose bowel movements.
If you are taking laxatives for constipation please tell the radiographers when you come for your planning scan.
The scan will be taken with you lying in the same position as for your treatment. The radiographers will draw some marks onto your skin, to be used as a reference for your treatment. You will then be scanned, which will only take a few minutes and at the end of the scan these marks will be replaced by permanent marks (tattoo), please see the picture below.
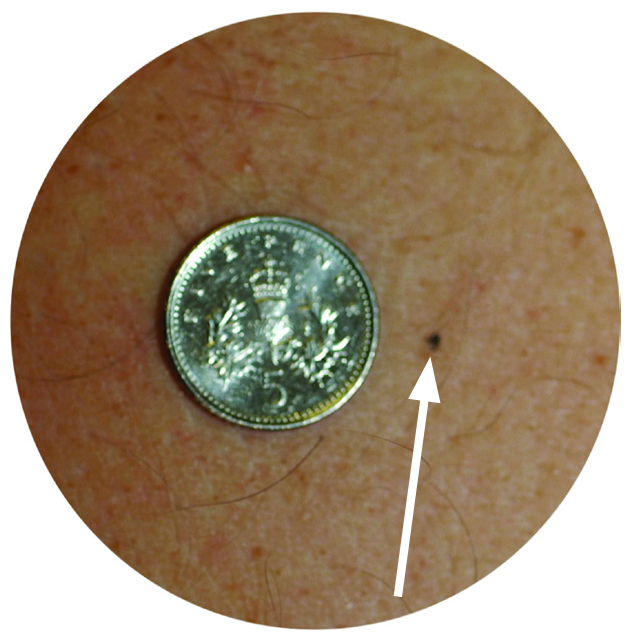
These permanent marks help us to ensure that you are in the same position each day. It also means that you can wash without worrying about your marks coming off.
Following the scan the radiographers will give you the time of your first appointment on the treatment machine. This is most likely to be a couple of weeks after your planning visit. The radiographers will talk to you about any further appointments you have.
Contrast (dye)
A special contrast agent, often called a dye, may be used for your scan to make specific organs, blood vessels and/or tissue types ‘stand out’. This can make it easier for the oncologist to plan your treatment.
The dye is given through a small needle into a vein in your arm. You should tell the radiographer if you have any allergies, but they will go over this before they use any dye.
The radiographers will advise you about drinking plenty of fluid after your injection.
Side-effects of the contrast
You may notice a warm feeling throughout your body and have a metallic taste in your mouth. You may also feel as if you have passed urine. This will pass very quickly. There is a small risk of an allergic reaction to the injection, such as a skin rash, but very rarely may lead to other complications.
The staff in the radiotherapy department are highly trained to manage any complications.
You will be able to drive your car or go to work after your scan.
Having your treatment
When you arrive for your treatment you should go to the radiotherapy reception desk at the entrance of the radiotherapy department. On the first occasion you will be given all your appointments and be escorted to the waiting area for your machine.
The radiographers will explain what will happen, including your bowel and bladder preparation and answer any questions that you may have.
You may need to partly undress and put on a gown; the radiographers discuss this with you when you first attend the department.
The radiographers will position you, and adjust the treatment couch and machine to the correct positions. For the first few treatments and also intermittently during treatment we will also take images to check the accuracy of the treatment which will take a few more minutes.
These images do not monitor your condition but are purely for treatment accuracy.
You will be asked to stay as still as possible during the treatment but you should breathe and swallow normally. Once you are in the correct position the radiographers will leave the room to switch on the machine. You will only be alone for a few moments at a time. The radiographers will be watching you on a closed circuit TV (CCTV) monitor during treatment. The CCTV camera is not recording or saving any images. There is also an intercom system so the radiographers can talk to you.
If you would like to listen to music during your treatment please let us know.
The treatment only takes a few minutes but you will be in the treatment room for about 10-20 minutes. The machine stops automatically after your prescribed dose of treatment has been given. The radiographers can stop the machine at any time if needed. The treatment machine makes a buzzing sound when switched on. You do not feel anything.
The radiographers may need to come in and out part way through each treatment.
After the treatment is complete the radiographers will come back into the room and help you off the couch.
On some days the radiotherapy department may be busy and there may be a delay before your treatment. We will keep you informed of any delays, please see the delay signs in the waiting areas. It may be a good idea to bring something to eat and drink with you, including any supplement drinks you have been asked to have and any medication you may need. There is a restaurant and café available on Level 0.
Your treatments will generally be on the same machine, although there may be days when this machine is being serviced and your treatment will be in a different room.
During your treatment we recommend you drink about two litres of fluid each day. This is the same as 3½ pints or about eight glasses.
If you have a kidney problem and drinking this amount of fluid would be difficult for you please inform your radiographer, nurse or doctor.
It is very important that you do not miss treatment days as it may make your treatment less effective. If you feel you are unable to attend for any reason please telephone us so that we can discuss this with you. If you have any queries about your appointment times please discuss these with the radiotherapy co-ordinators on your treatment unit.
For appointment queries please telephone the radiotherapy reception desk 0113 206 8940 for further advice.
Side-effects of treatment
Side-effects can be divided into short term (acute) effects, that happen during or soon after treatment, and long term effects occurring months or years later. Some side-effects are common, whilst others are rare. The area and amount of treatment given to you will affect which side-effects are most likely to happen to you. Your oncologist will discuss this with you. If you develop any radiotherapy side-effects you will be given advice and support by your healthcare team.
Short term side-effects from radiotherapy
Most side-effects are common and are temporary. They start during radiotherapy or shortly after completing radiotherapy. Usually they resolve within two to six months of finishing radiotherapy.
Tiredness
Nearly all patients having radiotherapy will feel tired. Be prepared to take things easy during treatment and allow for extra rests. There is a Macmillan information leaflet available and if you would like a copy, or support with your tiredness please ask a member of staff.
Tiredness usually improves in the weeks to months after treatment.
Things you can do to help include:
- Gentle exercise can help reduce the symptoms of tiredness.
- Having enough to drink can prevent tiredness from dehydration.
- Small meals or snacks eaten more often than three times a day may be easier to face.
- Try to get a good night’s sleep where possible, a daytime nap may help.
- Try to ‘pace’ yourself, listen to what your body is telling you, rest if you need to.
- Pick out the things that you enjoy, and try to accept help for some other tasks.
- Little and often is the rule of thumb.
Skin reaction
The skin in the treated area can become inflamed and sore about 10 days after the start of radiotherapy treatment. It may become dry and itchy. Sometimes later in treatment it may peel and become weepy. You may experience vaginal soreness and vaginal discharge.
Avoid hair removal in the treatment area where possible. This includes shaving, waxing, cream and lasers unless advised otherwise by your consultant, nurse or radiographer.
Before you go in for your treatment the radiographer will explain what will happen to your skin and how to look after it. They will also give you a leaflet to take home. If you are concerned about your skin reaction please talk to your radiographers or contact the review clinic nursing staff in the Princess Royal Suite, telephone: 0113 206 7587
Hair loss
Only hair in the treated area will stop growing and may fall out. Your doctor will tell you if you might lose your hair. Sometimes hair will not grow back after treatment.
Urinary problems
You may experience disturbance of bladder habit (when you are having a wee) with any of the following:
- urinary frequency: passing urine more often than normal
- urgency: a sudden urge to pass urine
- cystitis: pain on passing urine
- haematuria: passing blood in the urine.
Please let the doctor or radiographers know if you develop any of these symptoms. You may need a urine test to make sure that you do not have an infection.
You may need medication such as pain killers or antibiotics to help these symptoms.
You are advised to avoid coffee (caffeine) and alcohol. You should drink plenty of clear fluids and we advise drinking cranberry juice may also help.
Some fruit juices might interfere with the way some medicines work so please discuss this with your doctor or pharmacist before starting to drink cranberry juice.
Some patients may find that they have mild incontinence for a few months after the treatment. We would advise using incontinence pads which are available from your local chemist. If you are finding incontinence a problem please contact your team (Doctor or specialist nurses) or your GP for advice.
Bowel problems
You may experience disturbance of bowel habit with any of the following:
- Bowel frequency: opening your bowels (having a poo) more often than normal
- Urgency: a sudden urge to open your bowels
- Looser stools (looser poo) with more mucous or wind compared to normal
- Abdominal (tummy) discomfort which can be colicky (aching or cramping)
- Pain on opening bowels
- Bleeding from your back passage
- Pain from the skin on passing urine
- Rectal pain / discomfort
- Tenesmus: the sensation where you feel you need to open your bowels even if you have just done so.
Managing bowel problems
Diarrhoea can be managed effectively with medication (for example loperamide). You may need to stop using the micro- enemas.
Abdominal discomfort may be managed with medication to reduce the bowel spasms or cramps.
Tenesmus can be controlled with steroid suppositories or ointments which also contain an anaesthetic (such as Proctosedyl). Anti-constipation medicines may also help.
Wind/gas from the bowel
After radiotherapy you may find that you pass wind more often and have less control of when this happens. There can be many reasons for this:
- eating too many vegetables (see below)
- food containing starch and dietary fibre
- some medication used to regulate bowel habits.
Foods that may cause wind include:
- pulses (such as peas, beans and lentils)
- vegetables from the brassica family (such as Brussels sprouts, cabbage and artichokes)
- onions
- high-fibre food such as bran
- fizzy drinks.
If you are finding excess wind a problem please ask your clinical nurse specialist for advice.
Macmillan toilet card
If you want to go to the toilet more often, or feel that you can not wait when you do want to go, you can get a card to show to staff in shops, pubs and other places.
The card allows you to use their toilet without them asking awkward questions. You can get the cards from your radiographer or the information lounge in the radiotherapy department.

Loss of appetite
Your appetite may vary during your treatment. Try to eat well during your treatment and also drink about two litres of fluid each day. There are leaflets available, please ask a member of staff if you would like a copy.
When radiotherapy has finished
Your side-effects may get worse in the first few weeks after treatment and will then gradually settle. You should start getting back to normal about 4-6 weeks after treatment but it may take a little longer. Tiredness can last for several months and you may need to continue to rest more than usual.
You may be asked to attend the hospital where you were first seen by your oncologist for follow-up checks at regular intervals. This will vary according to the area you have had treated. Please discuss this with your doctor if you have any concerns.
Smoking
Smoking can have a significant impact on the side effects of treatment and can impact on the effectiveness of treatment.
Please contact your team about where you can get advice on stopping smoking.
Late effects of radiotherapy
Potential late effects from radiotherapy may happen many months or years after the treatment and may be permanent.
Bowel problems
- Bowel frequency: opening your bowels more often than normal
- Urgency: a sudden urge to open your bowels
- Looser stools compared to normal
- Increased wind
Bladder problems
- Urinary frequency: passing urine more often than normal
- Urgency: a sudden urge to pass urine
- Urinary incontinence: including urine leaking when coughing or straining
- Cystitis / pain when you pass urine
- Reduced bladder capacity
Local skin changes
- Skin thickening, thinning or discolouration
- Visible blood vessels
Vaginal changes
- Narrowing, shortening or dryness. This may impact on sexual function and comfort during examination. You may be advised to use vaginal dilators after treatment which may reduce this risk. Please refer to the paragraph ‘Vaginal dilators’ further on in this leaflet.
Pelvic bone fractures (hairline fractures of your pelvic bones)
- These may be asymptomatic or may cause symptoms. Pain can be managed with medicines.
Early menopause and infertility
Radiotherapy to the pelvic area usually involves the ovaries. Egg and hormone production will stop. You may develop symptoms of the menopause during or shortly after radiotherapy.
In pre-menopausal patients this can induce (bring on) an early menopause. Periods will stop and symptoms of the menopause may occur. If you have severe menopausal symptoms please discuss this with your oncologist or GP. They may recommend hormone replacement.
Infertility
If the radiotherapy area treated involves your pelvis or your ovaries then you will no longer be able to have children or carry a pregnancy in your uterus (womb) after radiotherapy. It is important that you use barrier contraception (condoms) during radiotherapy and for six months afterwards. If this is a concern or you are unsure if treatment will affect your fertility please speak to your doctor or nurse before starting treatment.
The symptoms of early menopause can include:
- Hot flushes and sweats
- Vaginal dryness
- Passing urine more often
- Lower interest in sex
- Tiredness and difficulty sleeping
- Dry skin
- Aches and pains
- Mood swings, poor concentration, lower confidence and changes in memory.
You may find the above symptoms affect your sex life in
some way.
Less common late side effects
Bowel / bladder damage
- May require surgery due to stricture (narrowing) or fistula (abnormal connection between two parts of your body) and may require stoma formation.
Lymphoedema
- Fluid build-up in your legs or pubic area.
Neuropathic pain or risk of nerve damage
- Pain due to irritation of nerves.
Risk of further cancer
Radiation treatment can cause a separate cancer in the years after treatment. These cancers most commonly occur in the organs next to the area treated, such as the rectum and bladder. At 10 and more years after treatment the risk of developing a second cancer is approx 1-2% (a cancer will develop in 1-2 people out of a 100).
Sexual intercourse
Patients who have had cancer have told us that it affects how you feel about your body, and can change your sex life. If you want, you can talk about these things in private with your key worker/clinical nurse specialist, or you can contact one of the organisations listed later in this leaflet for support. Macmillan also has some useful booklets that deal with these issues.
You can have sexual intercourse during radiotherapy if you feel comfortable. If having penetrative sex, you should use a barrier form of contraception e.g. condoms. Anxiety and worries about your illness and the future may cause you to lose interest in sex.
Although you may not feel able to have sex there may still be a need to express love and support. Talking with your partner may be helpful. You can resume sexual intercourse when you feel comfortable, this may be quite some time after your treatment has finished.
Cervical screening
Please discuss with your oncologists if you still need to attend your GP practice for smear tests or if you can be removed from the national register.
Vaginal dilators
Radiotherapy to the pelvis can cause a change in the vaginal tissue, which leads to a narrowing and shortening of the vagina. This is sometimes called ‘vaginal stenosis’. The vagina may become less elastic, drier and tender. This sometimes makes sexual intercourse and pelvic examinations difficult and painful. Using a dilator regularly after treatment will keep the vagina open and the tissues more supple. It will also make future vaginal / cervix examinations and penetrative sex more comfortable. Water-based or silicone-based lubricating gel can be used to help the dryness and can be used with the dilator or when having sexual intercourse.
You should begin to use dilators as soon as you feel comfortable which is usually 2-4 weeks after finishing treatment. Try not to delay starting using the dilators, as narrowing of the vagina is easier to prevent the earlier you start to use the dilators. We would advise and encourage you to use the dilators for the first two years after you have completed your radiotherapy. A member of the radiotherapy team will discuss this in more detail at the end of your treatment.
Pelvic Floor Exercises
You may have a more urgent need to use the toilet and difficulty in holding your bladder and bowels. This is because radiotherapy affects the muscles in your pelvic floor which are used when controlling your urges to pass water or stools. Doing pelvic floor exercises 3-4 times per day will help to strengthen these muscles and improve these side effects.
An information booklet called ‘Vaginal care after pelvic radiotherapy’ will be given to you and gives extra information about dilators and pelvic floor exercises.
Please ask for a copy if you have not been given one.
Research at Leeds Cancer Centre
Leeds Cancer Centre is a major centre for cancer research. You may be asked if you would like to help with some of the clinical studies. You are under no obligation to take part in any trials, and your treatment will not be affected in any way if you do not wish to take part.
If you do take part in a clinical trial you may meet a research nurse or radiographer who will be helping to run the trial.
Further information and support
If you have any questions please ask your hospital team. We all have our own ways of coping with difficulties.
Some people have a close network of family and friends who provide emotional support. Others would rather seek help from people who are not involved with their illness.
The following are also available as sources of information and support that you may wish to use.
Clinical Nurse Specialists (CNS)
Your CNS is available to discuss any aspect of your treatment with you. You will be seen by a CNS before your treatment. This is to offer support and advice about the practicalities and effects of your treatment and answer any questions you may want to ask.
Your CNS will also assess and discuss any physical, psychological, social, occupational and spiritual needs that you may have.
They can refer you to other services if needed, for instance, benefits advice.
You should be given a ‘key worker’ as a contact for support through your treatment; this is usually your CNS.
Macmillan Specialist Radiographer and Macmillan Radiotherapy Nurse Specialist
Sometimes people need more help if they are feeling depressed, very anxious or are having problems with their Radiotherapy. If this is the case you may benefit from seeing the Macmillan radiographer or nurse specialist, also known as the Radiotherapy patient support team.
Your oncologist, radiographer or nurse can refer you at any point before or during your treatment.
Local Support Services
Leeds Cancer Support
Leeds Cancer Support complements care provided by your clinical team. We offer access to information and a wide range of support, in a welcoming environment for you, your family and friends.
We can be found in the information lounges in Bexley Wing and also in the purpose built Robert Ogden Macmillan Centre (behind the Thackray Medical Museum).
The Sir Robert Ogden Macmillan Centre
This centre offers a variety of free health & wellbeing and supportive therapies for patients, their family members and carers. These include hypnotherapy, mindfulness coaching, acupuncture (for hot flushes) and pilates.
Contact numbers for Leeds Cancer Support
Information Lounge Level -2 Radiotherapy Department
Open from 8.00am – 6.00pm Tel: (0113) 206 7603
Information Centre Level 1 Outpatients Department
Open from 9.00am – 4.00pm. Tel: (0113) 206 8816
Sir Robert Ogden Macmillan Centre
Open from 9.00am – 4.00pm. Tel: (0113) 206 6498
All the above services can be emailed on:
leedsth-tr.cancersupport@nhs.net
Maggie’s Centre
If you or someone you love has cancer you may have lots of questions. Maggie’s is a warm, welcoming place where you can meet people who are experiencing similar things to you.
You may also be able to find support groups specific to your needs and get advice and information from their professional staff.
You don’t need an appointment and all support is free.
Open Monday to Friday 9.00 am – 5.00pm. Tel: 0113 457 8364
Address: St James’s Hospital (next to the multi storey car park), Alma Street, Leeds LS9 7BE
Email: leeds@maggies.org
Website: www.maggies.org
National Organisations
Jo’s Trust
Gives support for people with cervical cancer.
Tel: 0808 802 8000
Website: www.jostrust.org.uk
Ovacome (ovarian cancer support)
Support line for people with ovarian cancer and offers a range of information.
Tel: 0800 008 7054
Website: www.ovacome.org.uk
Target Ovarian Cancer
Gives information, materials and runs courses to support people with ovarian cancer.
Tel: 020 7923 5470
Website: www.targetovariancancer.org.uk
Lymphoedema Support Network
Tel: 020 7351 4480
Website: www.lymphoedema.org
Macmillan Cancer Support
This is a free telephone helpline to answer any questions you may have about living with cancer. They have a range of information dealing with emotional, practical and financial problems.
Freephone 0808 808 0000 – 8am to 8pm, seven days a week.
A textphone service for deaf and hard of hearing people is available on 18001 0808 808 0000.
Website: www.macmillan.org.uk
College of Sexual Relationship Therapists
Contact if you have sexual problems as a result of cancer. Lists of therapists are displayed on their website.
Tel: 020 8106 9635
Email: info@cosrt.org.uk
Website: www.cosrt.org.uk
Live Through This
A cancer support and advocacy charity for the LGBTIQ+ community.
Email: contact@livethroughthis.co.uk
Website: https://livethroughthis.co.uk
Relate
Gives advice, relationship counselling, sex therapy, workshops, meditation, consultations and support. You can choose to meet them face to face or via their website.
Email: relate.enquiries@relate.org.uk
Website: www.relate.org.uk
Stopping smoking
NHS Free Smoking Helpline – Monday to Friday 9am to 8pm, Saturday and Sunday 11am to 4pm.
Tel: 0300 123 1044
Website: www.nhs.uk/smokefree
Refreshments
A restaurant is available serving drinks, light snacks and hot meals. There is also a Café for hot drinks and light snacks; both of these are on Level 0.
Vending machines are also available on Level -2, Level 0 and Level 1. There is also a shop on Level 0 with books, papers and snacks.
Hotel Bexley Wing
The hotel is located on the 8th floor of Bexley Wing and offers 19 twin rooms and one single room. All have en-suite, tea and coffee making facilities, a mini-fridge, towels, hairdryer and digital television. There are two rooms with wheelchair access and a wet room.
Patients are able to stay free of charge. There is a charge for relatives if they are staying in their own room.
There are no cooking facilities in the hotel. The Bexley Wing Canteen is open Mon – Fri (closed during weekends) for you to purchase breakfast and lunch. This canteen closes at 3.00pm Mon – Thurs, on a Friday it closes at 2.00pm.
For more details please contact the Hotel Co-ordinator,
Mon-Fri 8.00am – 4.00pm on 0113 206 7687.
Car Parking
If you are coming by car follow the signs for St James’s Hospital, Bexley Wing. There is a drop-off point in the Plaza outside the main entrance and parking in the multi-storey car park next to Bexley Wing. There is a pedestrian walkway from the car park leading to the main entrance.
When you are coming for radiotherapy planning and treatment your car parking is free in the on-site multi-storey car park. Please ask a member of staff for more information about this.

This leaflet is under review and has been approved for a temporary print run from 10/10/2024 MIS:20241007_012/EP
A further extension has been approved until 16/04/2025 – JG