This leaflet aims to explain what happens when you have brachytherapy using temporary implants to treat your prostate cancer.
If you are visiting your GP, or other healthcare professionals, with any problems you may be having because of your prostate treatment, it may be helpful to take this booklet with you.
Each person’s treatment will vary, so the information given is a general guide. The healthcare team looking after you will explain your treatment and the side-effects in detail. If you have any questions after reading this leaflet, please speak to the team looking after you or ring the numbers at the end of leaflet.
Staff will make every effort to meet your individual needs or will direct you to the person who can help.
What is brachytherapy?
Brachytherapy is a form of radiotherapy given by directly introducing a radiation source into the area we wish to treat.
In the case of the prostate gland we do this with either permanent implants of radioactive iodine ‘seeds’ or temporary implants using applicator needles which are used to direct a radioactive iridium pellet into the prostate gland.
Treatment with temporary implants may be recommended as the best means of delivering high dose radiation to the prostate gland, in combination with external beam radiotherapy.
Is it suitable for all patients with prostate cancer?
No. It is suitable for patients who have localised prostate cancer or where there may be early spread into the nearby tissues. This risk is assessed by the size of the prostate gland on examination, the type of cancer cell (Gleason grade) and the Prostate Specific Antigen (PSA) level.
If you are taking aspirin or other blood thinning drugs, you will need to stop these before the implant to reduce the risk of excessive bleeding. You will be given further instructions by your consultant.
Will I have conventional radiotherapy as well?
Some patients may have a single implant treatment followed two to three weeks later by a three or four week course of external beam treatments given daily as an out-patient. Other patients may only have the brachytherapy treatment. Your doctor will discuss this with you.
What will happen during the brachytherapy treatments?
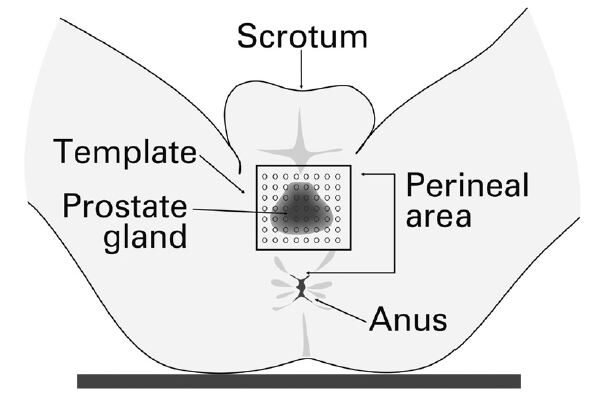
You will be admitted the morning of the procedure. You will be given an enema to clear your bowel, this makes the implant procedure easier. You will also be given an oral antibiotic to reduce the risk of infection. You will be taken to the brachytherapy treatment room and given a general anaesthetic. Whilst under anaesthetic fine needles will be passed into your prostate gland, guided by a trans-rectal ultrasound scanner. You will feel nothing whilst this is happening.
There will be a catheter (fine flexible tube) draining urine from your bladder. This will have been inserted before the implant takes place whilst you are under anaesthetic.
The radiation treatment is given in the brachytherapy treatment room whilst you are under anaesthetic. The needles are connected to a series of tubes which join them to the machine containing the radioactive pellet. Once this is completed, the staff leave the room, and the treatment will start (they will be watching you on camera at all times).
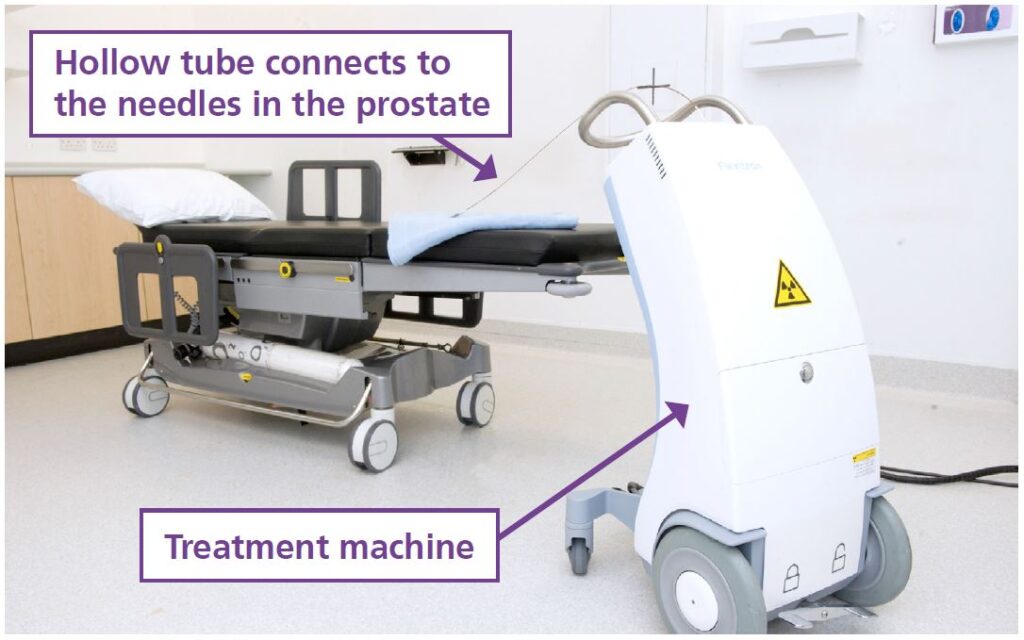
The machine will pass the pellet down each needle in turn, for the calculated length of time that is needed to deliver the necessary radiation dose. This is usually about 20 minutes in all. At the end of the treatment, the connecting tubes are removed from the needles. The needles will then be removed. You will be under general anaesthetic and feel nothing whilst treatment is delivered. At the end of the anaesthetic you will be given a blood thinning injection to reduce the risk of Deep Vein Thrombosis (DVT).
When you wake up from the anaesthetic
When you come round from the anaesthetic you will return to the ward, you will be admitted to one of the oncology wards where you will be monitored overnight. The catheter draining your bladder will be removed on the ward, unless we have reason to be concerned about your ability to pass water. You may pass small amounts of blood in your urine for a few days after the procedure. There is no need to worry about this. We advise you drink two to three litres of water per day to help with these symptoms.
Tea, coffee and coca-cola, contain caffeine and can have an effect on your urine output. It is advisable to avoid these until your bladder irritation settles. You can have decaffeinated drinks.
You may feel a little bruised in the area of the skin between your scrotum and your anus. Most patients do not experience much discomfort. You will be given painkillers if you need them.
Is there anything else I should know?
The area where the implant was placed may feel a little uncomfortable for a few days, particularly if you sit on a hard chair.
Sometimes bowel movements may feel uncomfortable for a few days and may occasionally cause a sharp pain in that area. This settles on its own and is rarely enough to need active treatment.
You will also be given Tamsulosin (Flomax®). This is an alpha-blocker tablet which relaxes the smooth muscle of the urethra (the tube that leads from the bladder through the prostate and penis) and helps urination. It is recommended you take one daily until symptoms settle.
After a few weeks you should find that you can return to your normal level of activity. You may eat whatever you like after the treatment.
Your clinical team contacts
Your Clinical Nurse Specialist (Leeds patients only)
0113 206 6792
Dr Bottomley
Secretary 0113 206 8986
Prof Henry
Secretary 0113 206 8986
Dr Rodda
Secretary 0113 206 7630
Dr Dugdale
Secretary 0113 206 8986
Support Services
Leeds Cancer Support
Leeds Cancer Support complements care provided by your clinical team. We offer access to information and a wide range of support, in a welcoming environment for you, your family and friends.
We can be found in the information lounges in Bexley Wing and also in the purpose built Sir Robert Ogden Macmillan Centre.
The Sir Robert Ogden Macmillan Centre
This centre offers a variety of free health & wellbeing and supportive therapies for patients, their family members, and carers. These include hypnotherapy, mindfulness coaching, acupuncture (for hot flushes) and pilates.
Live Through This
A cancer support and advocacy charity for the LGBTIQ+ community.
Email: [email protected]
Website: https://livethroughthis.co.uk
Maggie’s Centre
If you or someone you love has cancer you may have lots of questions. Maggie’s is a warm, welcoming place where you can meet people who are experiencing similar things to you. You may also be able to find support groups specific to your needs and get advice and information from their professional staff.
You don’t need an appointment and all support is free.
Open Monday to Friday 9.00 am – 5.00pm. Tel: (0113) 457 8364
Address: St James’s Hospital (next to the multi storey car park), Alma Street, Leeds LS9 7BE.
Email: [email protected]
Website: www.maggiescentre.org
National Support Organisations
Macmillan Cancer Support
Freephone: 0808 808 0000, 8.00am to 8.00pm seven days a week.
A textphone service for deaf and hard of hearing people is also available.
Textphone: 18001 0808 808 0000
Website: www.macmillan.org.uk
Prostate Cancer Charity
Freephone: 0800 074 8383
Website: www.prostatecanceruk.org
