This leaflet also includes information on vasa praevia (blood vessles from your baby to the placenta pass near to the cervix). In this leaflet you will find information on what a placenta praevia, placenta accreta and vasa praevia mean and what to expect throughout your pregnancy, how your pregnancy will be monitored and how to seek advice. If you have any concerns or questions please speak to your midwife who will be able to advise you further.
What does placenta praevia mean?
Along with a baby, a placenta develops in the uterus (womb) during pregnancy. The placenta provides oxygen and nutrients from the parent’s blood stream. The placenta is is delivered after the birth of baby and is also known as the afterbirth.
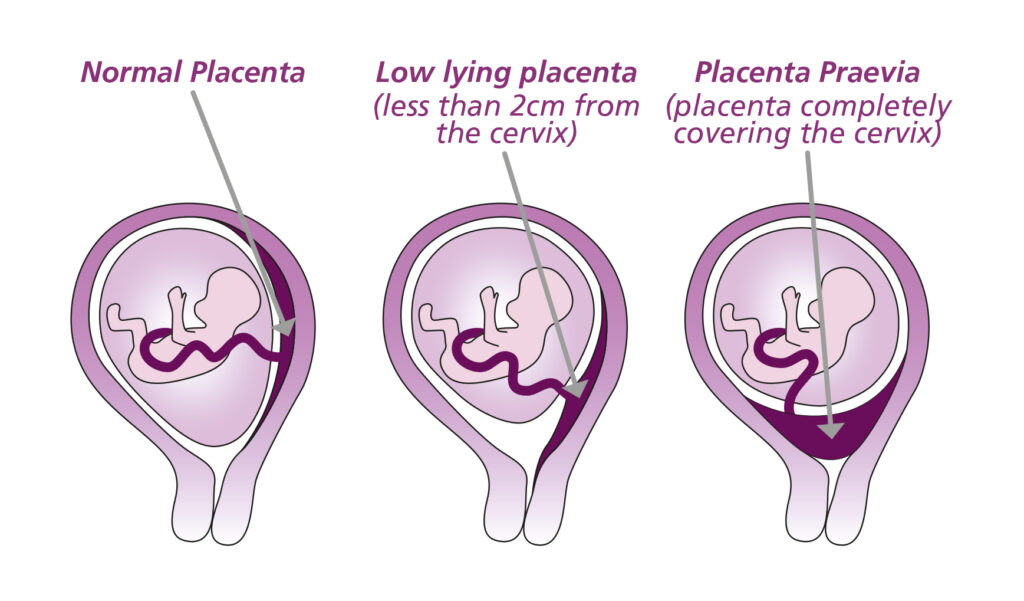
A placenta praevia means the placenta is on the lower part of the womb, near to or covering the cervix (neck of the womb). A placenta praevia may also be referred to as a low lying placenta.
As many as 1 in 20 pregnancies will have a low lying placenta which is usually found at the 20 week scan. As the pregnancy progresses and the womb grows the placenta moves up out of the way of the cervix and is no longer classed as low lying.
How will I know if my placenta is still low lying?
You will be invited to attend another scan later on in your pregnancy, to check the location of your placenta.
You will be invited to have a scan around 32 weeks pregnant if you have had one or more previous caesarean section, or if your placenta is completely or partially covering the neck of the womb.
You will be invited for a further scan at 34 weeks pregnant if your placenta was less than two centimetres from the neck of the womb.
A trans-vaginal scan may be necessary as this allows a better view of the placenta’s location. A trans-vaginal scan is where a small scan probe is gently placed inside your vagina. It is completely safe for you and your baby.
What if my placenta has moved?
If there is two or more centimetres between the edge of the placenta and your cervix (neck of the womb) this is normal and no further investigations are needed.
What if my placenta has not moved?
If your placenta has not moved at the 32-34 week scan, arrangements will be made for you to see a doctor that will discuss these findings with you.
One in 200 pregnancies will have a placenta praevia at the end of the pregnancy.
There is a risk that you may have vaginal bleeding, particularly towards the end of the pregnancy, because the placenta is low down in your uterus. Bleeding from placenta praevia can be very heavy, sometimes putting both you and your baby’s life at risk.
Your baby may need to be born by caesarean section because the placenta may block the birth canal, preventing a vaginal birth. In such cases it is recommended that your baby is born by elective caesarean section.
If you have placenta praevia, you are more likely to have your baby early (less than 37 weeks). For this reason you may be offered a course of steroid injections between 34 and 36 weeks of pregnancy to help prepare your baby’s lungs if they were to be born early.
Delivery is usually from 36-37 weeks and you may only be offered a course of steroids if required, and the risks and benefits will be discussed with you.
Additional care, including whether or not you need to be admitted to hospital for observation, will be based on your individual circumstances. Even if you have had no bleeding before, there is a small risk that you could bleed suddenly and heavily, which may mean that you need an emergency caesarean.
What precautions will I need to take?
You should try to avoid becoming anaemic during pregnancy by having a healthy diet and by taking iron supplements if recommended by your healthcare team. Your blood iron (haemoglobin) levels (a measure of whether you are anaemic) will be checked at regular intervals during your pregnancy.
If you have a low lying placenta there is a small risk you may bleed suddenly or heavily. This can be at any point in your pregnancy and not necessarily accompanied by pain.
It is important that you do not delay contacting the Maternity Assessment Centre in the event of any bleeding, pain or contractions, specifying that you have a low lying placenta/placenta praevia.
If you have bleeding, your doctor may need to do a speculum examination to check how much blood loss there is and where it is coming from. This is a safe examination and you will be asked for your consent beforehand.
What is a Placenta Accreta?
Placenta accreta is a rare complication of pregnancy affecting between one in 300 and one in 2000 pregnancies. A placenta accreta is when the placenta grows into the muscle of the uterus, making delivery of the placenta at the time of birth very difficult.
Placenta accreta is more common where a placenta praevia has been found, and when previous caesarean birth has happened, but it can also occur if you have had other surgery to your uterus (womb), or if you have a uterine abnormality such as fibroids or a bicornuate uterus. It is more common if you are older (over 35 years old) or if you have had fertility treatment, especially in vitro fertilisation (IVF).
Placenta accreta may be suspected during a pregnancy scan. If a placenta accreta is suspected you may be offered a magnetic resonance imaging (MRI) scan to help with the diagnosis. A placenta accreta is only able to be confirmed at the time of a caesarean section. MRI scans are safe in pregnancy as they contain no radiation.
If you have placenta accreta, there may be bleeding when an attempt is made to deliver your placenta after your baby has been born. The bleeding can be heavy and you may require a hysterectomy to stop the bleeding.
If placenta accreta is suspected before your baby is born, your doctor will discuss your options and the extra care that you will need at the time of birth and an individual management plan will be made. Depending on your individual circumstances you may require a caesarean section or your baby may be required to be born early between 35-37 weeks. Delivery is usually planned before you’re likely to labour
(34-36 weeks). If you start bleeding or having pain before this, you will be admitted as an emergency and may need delivery earlier.
You will need to have your baby in a hospital with specialist facilities available and a team with experience of caring for women with this condition such as in Leeds where we are a regional referral centre for abnormally invasive placenta.
It is important that you do not delay contacting the Maternity Assessment Centre in the event of any bleeding, pain or contractions, specifying that you have a placenta accreta.
If you have bleeding, your doctor may need to do a speculum examination to check how much blood loss there is and where it is coming from. This is a safe examination and you will be asked for your consent beforehand.
If you would like more information on placenta accreta speak to your doctor and they will be able to provide you with this and further patient information leaflets and resources.
What is vasa praevia?
Vasa praevia is a very rare condition affecting between 1:1200 and 1:5000 pregnancies. It is where blood vessels from your baby to the placenta pass near to the cervix. These blood vessels are very delicate and can tear when you are in labour or your waters break. This can be very dangerous as the blood that is lost comes from your baby. Babies only have a small amount of blood so do not need to lose much to become very unwell or even die.
It is important that you do not delay contacting the Maternity Assessment Centre in the event of any bleeding, pain or contractions, specifying that you have a vasa praevia.
If you have bleeding, your doctor may need to do a speculum examination to check how much blood loss there is and where it is coming from. This is a safe examination and you will be asked for your consent beforehand.
If you have been identified as having a vasa praevia you will be referred to a consultant for review and an individualised plan for your pregnancy and delivery will be made with you.
For more information please visit:
Or contact your community midwife.
References
- RCOG green top guideline n27
- “The Use of Ultrasound in Pregnancy including the Screening and Management of the Small for Gestational Age Fetus” Leeds Teaching Hospitals guideline.
- RCOG Patient Information Leaflet 2018 ‘Placenta praevia, placenta accrete and vasa praevia’