Sometimes the speed at which everything happens when the diagnosis of melanoma is made can feel overwhelming. You may feel as if you are in your doctor’s surgery one day and waking up after an operation the next.
This speed does not give you very much time to deal with your feelings in any depth. Sometimes you can only begin to think about the emotional issues after the initial treatment has been completed. It is only then that you are able to take the time and have the energy to begin to look at things in any detail.
Coping after a diagnosis
Some people worry that they do not know how to cope with a diagnosis of cancer. This is not surprising. The word cancer frightens nearly everyone. Most of us do not have past experience to draw on to help us and the speed and ever-changing challenges make it difficult to have a clear plan of action.
As there is no one standard set of reactions to the diagnosis, so there is no standard way of coping. We will all find our own way. For cancer patients in the long term, lack of certainty about the future is a common cause of anxiety. The Leeds Psychology Service in Bexley Wing is specifically designed to give support to patients dealing with cancer and if you are struggling then a referral to that service may well help.
However, there are some general points that you might find helpful. Difficult though it is, confronting and being open about your feelings is a good place to start.
It is often helpful to be able to share these feelings with a trusted friend – someone who is not going to tell you to pull yourself together or to stop being silly. The sort of friend who will listen without judging, be with you and not interrupt, to support without interfering. Simply ‘getting things off your chest’ is all that you may need. Some of you will find it helpful to talk to someone outside of your family or friends – your doctor or specialist nurse, a counsellor or psychologist. They are there to help you, to support you, so do not be afraid to ask if that’s what you think you need.
If you hear any words or phrases that you do not understand, please ask your doctor or a member of your healthcare team what it means. It does not matter how many times you ask.
Sun protection
It is sensible to reduce sun exposure for you and your family, because the main cause for melanoma is intense sun exposure on holiday or at weekends. Curiously regular moderate sun exposure does not seem to cause melanoma: It’s getting burnt in the sun which we think is the cause. Avoiding this sort of sun exposure is particularly sensible advice if you and your family are moley, especially if they have the Atypical Mole Syndrome (AMS) – lots of moles.
It is also particularly sensible if you and your family are fair skinned: if you burn in the sun, if you have red hair or freckles.
- The best advice for you and your family is to keep out of bright sun light but this does NOT mean you cannot go on holiday. Have fun but don’t let anyone in the family get burnt (and this includes going pink in the sun) and don’t sunbathe. You cannot undo the skin damage from the sun in the past but you might be able to prevent damage in your children and grandchildren.
- Keep out of the sun when it is most strong: between the hours of 11:00am and 3:00pm. Seek the shade then: have lunch. Arrange to go out early morning and late afternoon.
- Use the shade. Trees, umbrellas and buildings all give shade throughout the day from buildings as the sun moves round.
- Leave your shirt on! Avoid strappy tops which leave the shoulders exposed.
- Hats give good protection to the face, neck and ears (particularly important for people with short hair) if you are out in direct sunlight on a hot day. Four inch brims are desirable: the more popular baseball caps are less valuable because they do not protect the neck and ears. Out on a walk or working in the garden, hats are good.
- Sunblock is useful for the skin which cannot be covered, but it is not the be-all and end-all of sun protection. Use waterproof sun block with an SPF (Sun Protection Factor) of at least 30, and 4-5 stars UVA protection. Apply plenty of sunscreen 15-30 minutes before going out in the sun, and reapply every two hours, and straight after swimming. No sunscreen will provide 100% protection.
The sun is a very important source of vitamin D (which is crucial for health) so if you and your family are very careful in the sun you may need some vitamin D supplements: please see our leaflet on ‘Sun protection and Vitamin D’.
Advice about sun protection is available from the SUNsmart campaign www.sunsmart.org.uk
What else should I do to my lifestyle?
Patients often ask about diet and alcohol and reasonable advice would be to eat a healthy diet (as we should all do), with five or more portions of fruits or vegetables a day. A diet which is rich in these foods and contains less meat, sugar and fat is better for many aspects of health and is probably therefore better for cancer patients too.
Beyond that, moderation seems sensible advice but the maxim that ‘a little of what you fancy does you good’ also seems appropriate.
Exercise is also extremely important for health generally and is likely to be at least as important to cancer patients as it is to us all. The NHS Choices web site states the following:
‘To stay healthy, adults aged 19-64 should try to be active daily and should do: at least 150 minutes (two and a half hours) of moderate-intensity aerobic activity such as cycling or fast walking every week, and muscle-strengthening activities on two or more days a week that work all major muscle groups (legs, hips, back, abdomen, chest, shoulders and arms)’.
Smoking
In Leeds, we have found evidence that smoking at the time of diagnosis of melanoma increases the risk of melanoma recurrence. If you do smoke we would advise you to stop, although we do understand how difficult it might be. Your GP should be able to advise you as to the help available.
Some people react to the diagnosis of melanoma by reassessing their life and their life-style generally. Some try to achieve a ‘better balance’, which also seems sensible. Some decide to take that special holiday.
Looking after yourself
Examining your lymph glands
The lymphatic system
Lymph glands are part of the lymphatic system which is both a fluid drainage system and part of the immune system.
The system is made up of tiny channels called ‘lymphatics’. These channels drain fluid from the skin and other tissues back into the blood, passing the fluid through the lymph glands on the way. The lymph glands are part of the immune system: so movement of fluid is important in defending against infection and cancer.
However the commonest way that melanoma may spread is also within the lymphatic channels. Cells may travel within these channels settling in the nearest lymph gland where they can grow and show up as a swelling or lump. These lumps are enlarged lymph glands in which melanoma cells are growing.
The lymph gland in which a swelling is most likely to occur is to some extent predictable.
(a) Melanomas on the leg usually produce lumps in the groin.
(b) Melanomas on the arm usually produce lumps under the arm.
Melanomas on the trunk (back or chest) may produce lumps in the groin or under the arm.
(c) Melanomas on the head usually produce lumps in the neck.

What should I do if I develop swollen lymph glands?
If you think you have a swollen lymph gland, telephone your melanoma clinic or GP. Your Melanoma Specialist Nurse (sometimes called a key worker) is often the best person to call and they will arrange an appointment for clinic as soon as they can.
Often patients are feeling entirely normal glands, which have come up because they have had an infection, banged their toe etc.
Don’t worry at home: get the gland checked.
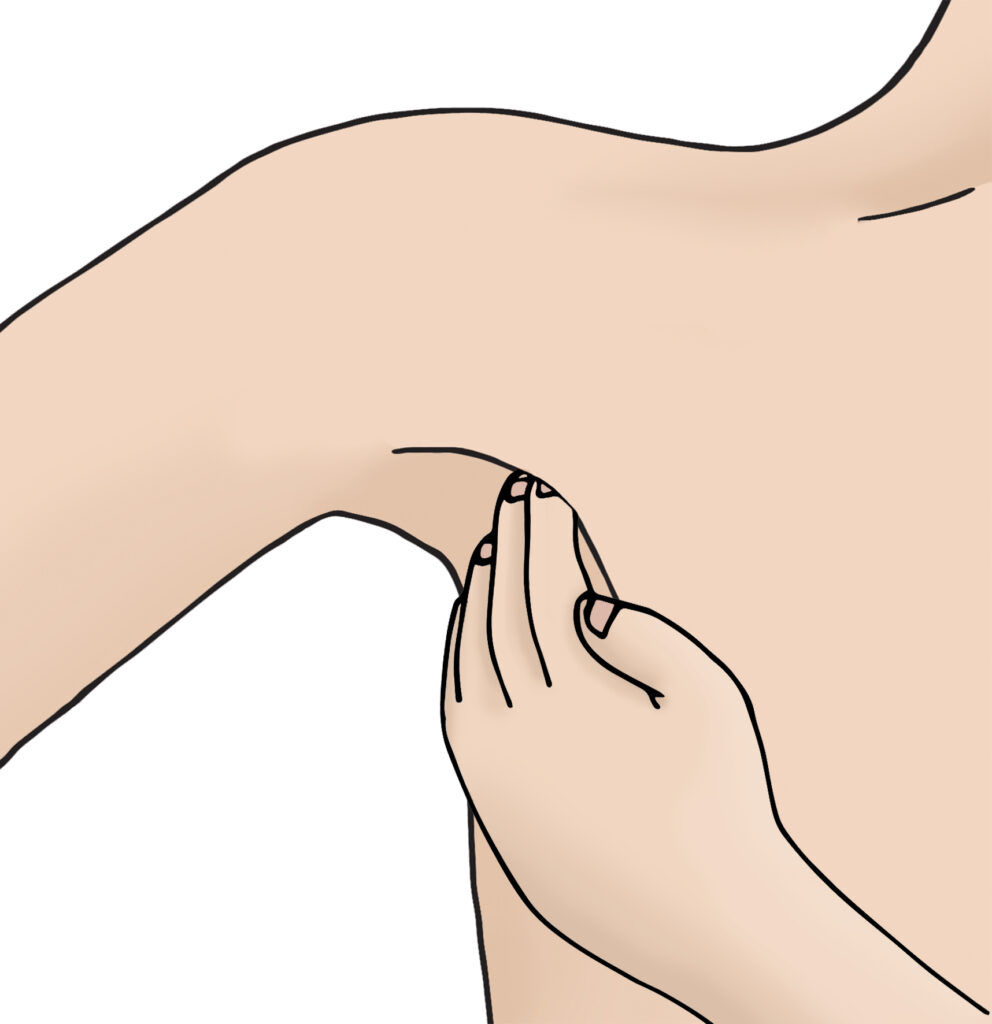
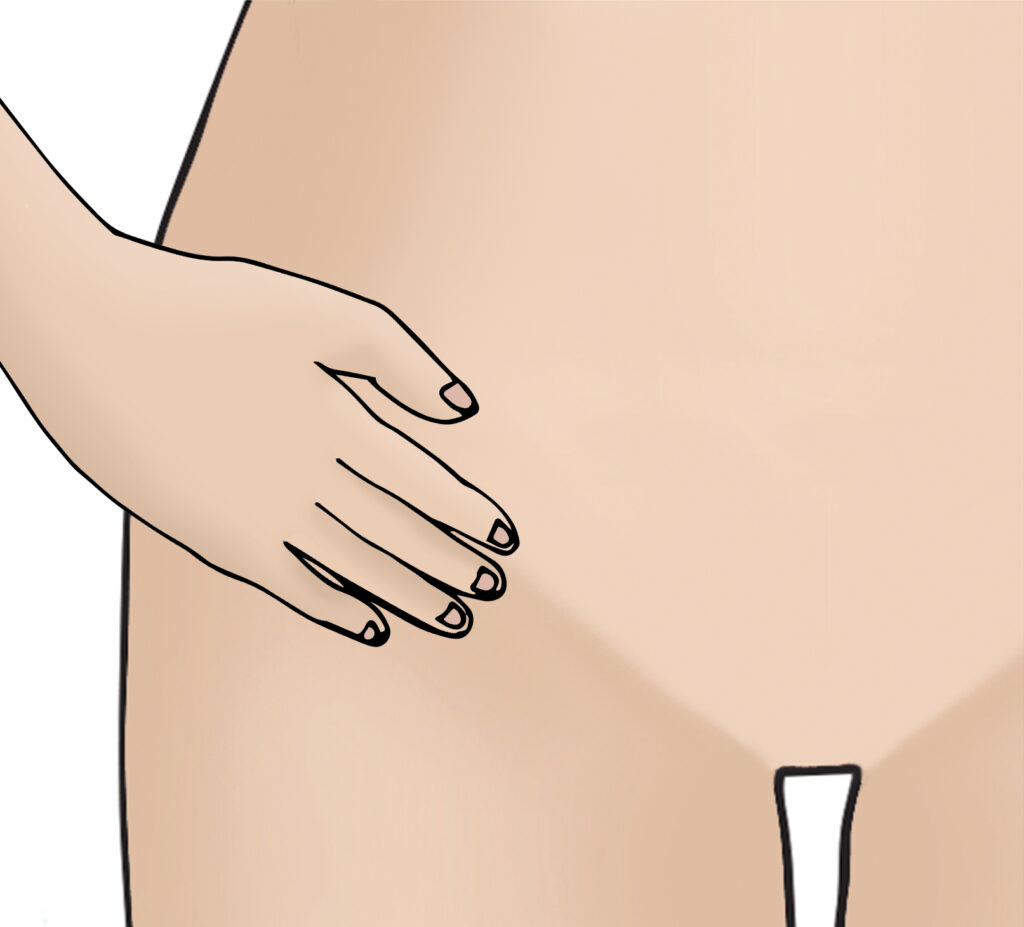
These images show how to examine lymph glands.
Frequently asked questions
Will I need other tests?
Will I need any tests after my operation?
After a melanoma has been removed from the skin, patients are followed up in clinic in order to pick up a recurrence (sometimes called a secondary) of that melanoma should it occur.
The majority of melanoma patients never have a recurrence, but some do. The most common place for the melanoma to recur is as a swollen gland as discussed on page 6 ‘Looking after yourself after Melanoma – Examining your lymph glands.’
The best way to find swollen glands is by physical examination. Follow up in clinic is usually by thorough examination rather than by tests such as scans.
Some patients will have a chest x-ray and a blood test. These tests may be used as a baseline so that later if you have symptoms (for example a cough) it will be helpful to have a previous chest x-ray to compare with. They are not however essential.
Is a routine scan required after my melanoma is removed?
Some patients seek the reassurance of a normal scan and it is reasonable to discuss this with your doctor.
However, scans can cause more trouble than they are worth. It is very unlikely that a scan will show any abnormality soon after a melanoma has been removed. The scan may however show minor abnormalities, which cause confusion. Around a quarter of people have cysts etc on their scan, which cause anxiety even though they are harmless.
This can of course be very worrying and it will need a second scan later to resolve the doubt.
Furthermore, body scans expose the body to a dose of radiation and should therefore only be used when there is good reason to do so.
In clinics we therefore usually try to carry out scans only when they are likely to be helpful rather than routinely.
Will I need any tests after my operation?
Scan – Summary
Generally speaking whether you should have a scan should be decided by you and your doctor, balancing the following:
- The risk of the melanoma coming back. Most melanoma patients have a low risk of the melanoma ever returning. If the risk is higher, for example if melanoma has developed in a swollen gland, then a scan may be sensible.
- The presence of any symptoms, such as sickness, or pain.
- The negative aspects of having a scan such as detecting harmless changes in a significant percentage of patients.
- The dose of radiation.
Follow up
It is routine practice to follow up patients in a hospital clinic in the UK for 1-10 years after diagnosis.
The frequency of follow up depends on what stage of melanoma you are. This will be explained to you at your appointments. It is not unusual for your follow up to be shared between different doctors.
The purpose of follow up is:
- To detect a recurrence of the melanoma, should it develop.
- To examine the skin and to teach patients how to monitor their own skin.
- To support the patient through diagnosis and afterwards.
Insurance
Buying insurance for travel or life insurance can be difficult after a diagnosis of cancer. Macmillan Cancer Support have good booklets about both, if you need these please ask your specialist nurse or look on the internet.
Our comments would be:
- Always declare the fact that you have had a melanoma. Patients do get into trouble regularly overseas when they are ill because of their cancer and cannot pay for treatment abroad or travel back home again.
- Shop around for insurance: again Macmillan Cancer Support have advice on line and your specialist nurse will also have access to information.
Critical illness mortgages and health insurance policies
After a diagnosis of cancer its worth considering whether you have any health insurance or critical illness policies which might trigger a payment. Again Macmillan Cancer Support has information about this in their booklet ‘Insurance’. Macmillan provides financial advice via the telephone.
Pregnancy
If you would like to have a baby after a diagnosis of melanoma its worth talking this through with your medical team before conceiving. There is no evidence that pregnancy increases the risk of melanoma recurring during pregnancy, but having secondary melanoma whilst pregnant makes treatment difficult. It is also possible (although extremely rare) for melanoma to pass from the mother to the baby in the womb. The advice to wait before conceiving is usually given, but the advice should probably be individual. Happily most young women diagnosed with melanoma have a low risk of recurrence of their melanoma, and waiting to conceive would make less sense for them. It would be sensible for women with more serious melanomas to wait at least for a few years. Please talk to your doctor or nurse specilaist for advice.
Free prescriptions
Patients being treated for cancer are currently entitled to free prescriptions. Patients can apply for an exemption certificate by collecting a FP92A form from their GP surgery or oncology clinic. The form must be countersigned by their GP or hospital doctor, then sent to the NHS Business Services Authority (BSA), who will issue an exemption certificate.
Patients can show their exemption certificate to their pharmacist as proof of exemption. The certificate will last for five years. Once the certificate has expired a new application can be made if treatment is continuing or patients are suffering the effects of cancer or its treatment. The NHS BSA will remind patients before the expiry date.
Resources
Useful web pages
For information about sun protection visit:
Cancer Research UK
For information about melanoma visit:
Cancer Research UK
Macmillan Cancer Support
BBC health information
The Cancer Counselling Trust
www.cctrust.org.uk
Marie Curie Cancer Care
NCRN
www.ncrn.org.uk
Melanoma Focus
The Melanoma Genetics Consortium
Organisation addresses
Cancer Research UK
PO Box 123, London WC2A 3PX