This leaflet is designed to help you look after your own moles. It is hoped that it will be useful for everyone but it may be especially valuable for people who are at increased risk of melanoma (a form of skin cancer).
Who is at increased risk of melanoma?
- People who have had a previous melanoma.
- People who have had other forms of skin cancer.
- People with a family history of melanoma. For more information see www.genomel.org/family
- People with many moles.
- People with many large and irregular moles, Atypical Mole Syndrome (AMS)
- People with fair skin (skin which burns easily in the sun), freckles and/or red hair.
- People who have had severe, blistering sunburns in the past.
What should I do?
Look at your moles once a month
Good light is needed and a partner is useful to examine areas such as the back and scalp. Become familiar with your moles so that you can recognise a change. If in doubt ask your doctor to check the mole.
Things to remember:
- If you have many moles you cannot be expected to monitor them all in great detail: you are looking for one that stands out from the crowd.
- Change usually occurs quite slowly over weeks and months so you have time to spot the development of the commonest type of melanoma: the superficial spreading melanoma.
- You are looking for changes in colour, size or shape.
- Normal moles do change as you get older. They often slowly become dome-shaped with age and lose their colour. Photographs of such moles follow on the next pages. It is important to know how moles change normally with time, to distinguish from worrying changes.
- As we get older we develop lots of lumps and bumps, which are harmless but can cause anxiety especially when you have had a melanoma. If in doubt, show your family doctor.
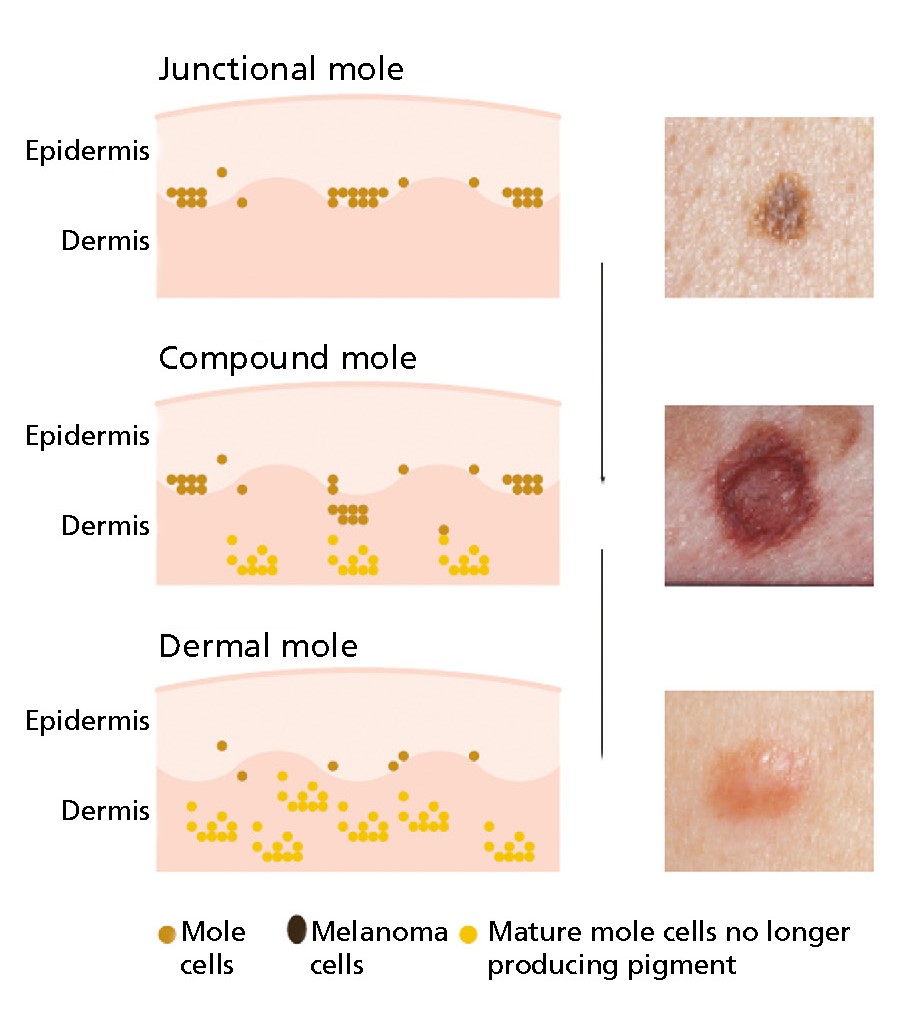
Normal changes in moles as you get older
When they first appear moles are flat and brown. However on some parts of the body they can develop a smoothly domed shape and return to the general colour of the skin. You may have seen examples of these mature moles around the mouths of elderly people from which hairs often emerge. These illustrations/photographs show examples of the changes in moles which occur normally as we get older.
Normal moles
Some doctors will give their patients close up photographs to help them monitor their moles.
Normal moles come in a variety of shapes and sizes and the following photographs show mature moles which are all benign (harmless).
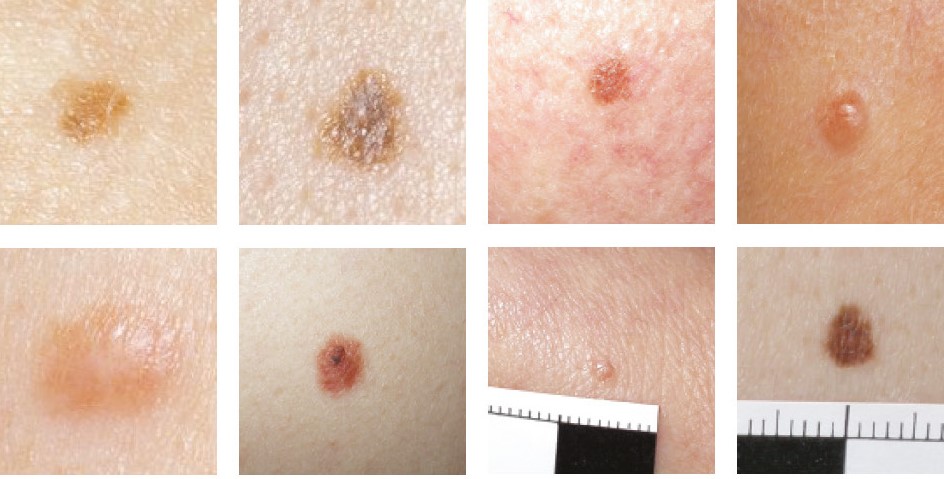
These photographs show normal variations in colour and shape.
The important thing is to learn how to spot changes.
Atypical moles
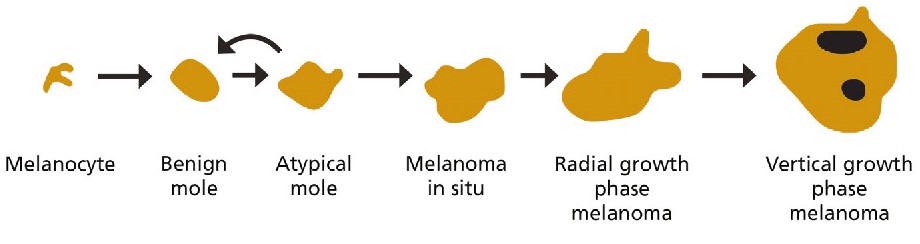
Atypical moles are moles which are bigger than usual and more irregular in shape and colour. Atypical moles are a little more likely to become a melanoma than others.
These are examples. Such moles should be shown to your doctor.




Atypical moles are somewhere between a benign mole and a superficial spreading melanoma. The illustration below shows how melanoma may develop over time from atypical moles.
However, most do not progress, but disappear as we get older.
Moles that become more irregular in shape and colour over time should be shown to your doctor to exclude melanoma.
Atypical Mole Syndrome
Some people have multiple atypical moles and are said to have the atypical mole syndrome (AMS). This is seen in about 2% of the population in the UK. Individuals with the AMS are considered to have a higher risk (increase 7-10 fold) of developing melanoma compared to the general population.
An individual atypical mole can be removed surgically if the dermatologist is concerned about it. However most of these moles will not require removal.
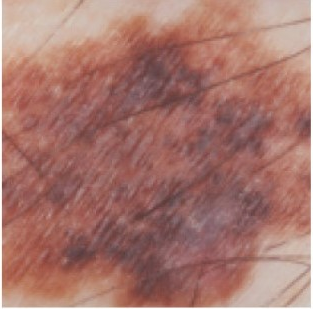
Melanoma in situ
Very early melanomas are known as melanomas in situ and the following photographs are good examples.
These melanomas are so early that removal should cure the patient entirely.


Superficial spreading melanomas
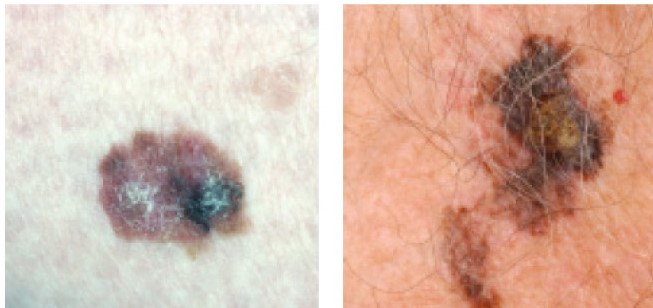
These are melanomas which initially grow laterally (sideways) in the epidermis. This is known as the radial growth phase.
These melanomas often grow in moles and in their early stages look like moles.
Removal of a radial growth phase melanoma by surgery should cure the patient. Otherwise, over time, the cancer cells start to grow downwards (vertical growth phase) into the dermis.
The thickness of a melanoma can be used to estimate further spread to other organs.
Early diagnosis and treatment, when melanomas are thin, is therefore very important.
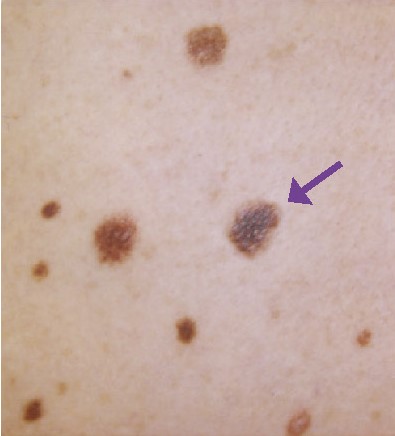
Odd one out
If people are very “moley” they cannot be familiar with all of their moles – it is useful to look for one that stands out in the crowd.
In this photograph the arrow shows the mole that is subtly different, and proved to be an in situ melanoma.
Sun Protection
The main cause of melanoma is intense sun exposure on holiday or at weekends. Avoiding getting sunburnt (this means going pink in the sun) and sunbathing
is particularly important.
The sun is a very important source of vitamin D so if you and your family are very careful in the sun you may need some Vitamin D supplements: please see our leaflet
‘Sun protection and Vitamin D’.
Glossary
Benign
A lump or growth, which is not cancer. These growths do not grow very quickly, and they do not spread to other parts of the body.
Cancer
A disease in which cells grow in an uncontrolled way. Such cells spread elsewhere in the body and, if they are not treated, interfere with the way the body functions or works.
Diagnosis
The name given to the illness that a person has.
Melanocytes
The cells that produce the dark pigment that gives skin and hair its colour.
Melanoma
A cancerous growth which may develop from normal skin or may grow from a mole.
Melanoma in situ
Very early melanoma, which remains entirely in the top layer of the skin (epidermis). This sort of melanoma is curable and should never come back.
Mole
A harmless or benign growth of pigment cells in the skin. The formal name for moles is naevi.
Resources
Useful web pages
For information about sun protection visit:
SunSmart
For information about melanoma visit:
Cancer Research UK
Wessex Cancer Trust
MARC’s Line
Macmillan Cancer Support
BBC health information
The Cancer Counselling
Trust www.cctrust.org.uk
Marie Curie Cancer Care
NCRN
www.ncrn.org.uk
Melanoma Focus
The Melanoma Genetics Consortium

