Why are stents inserted?
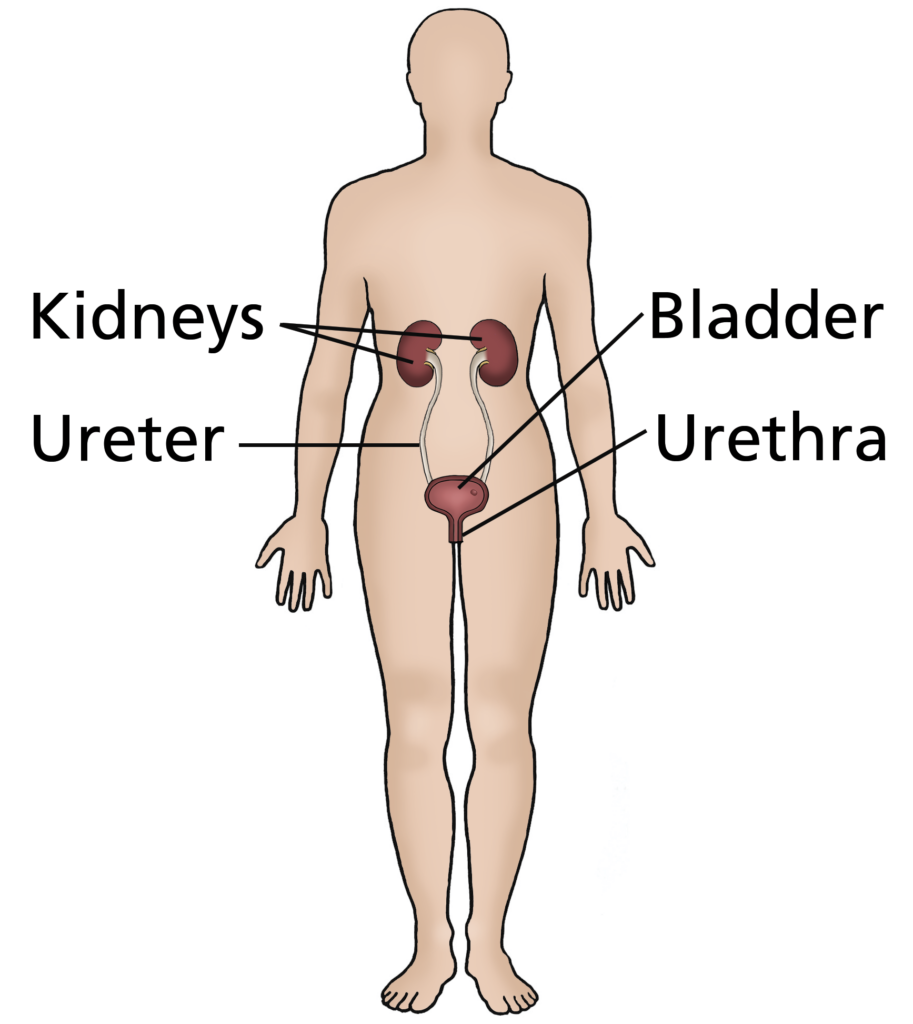
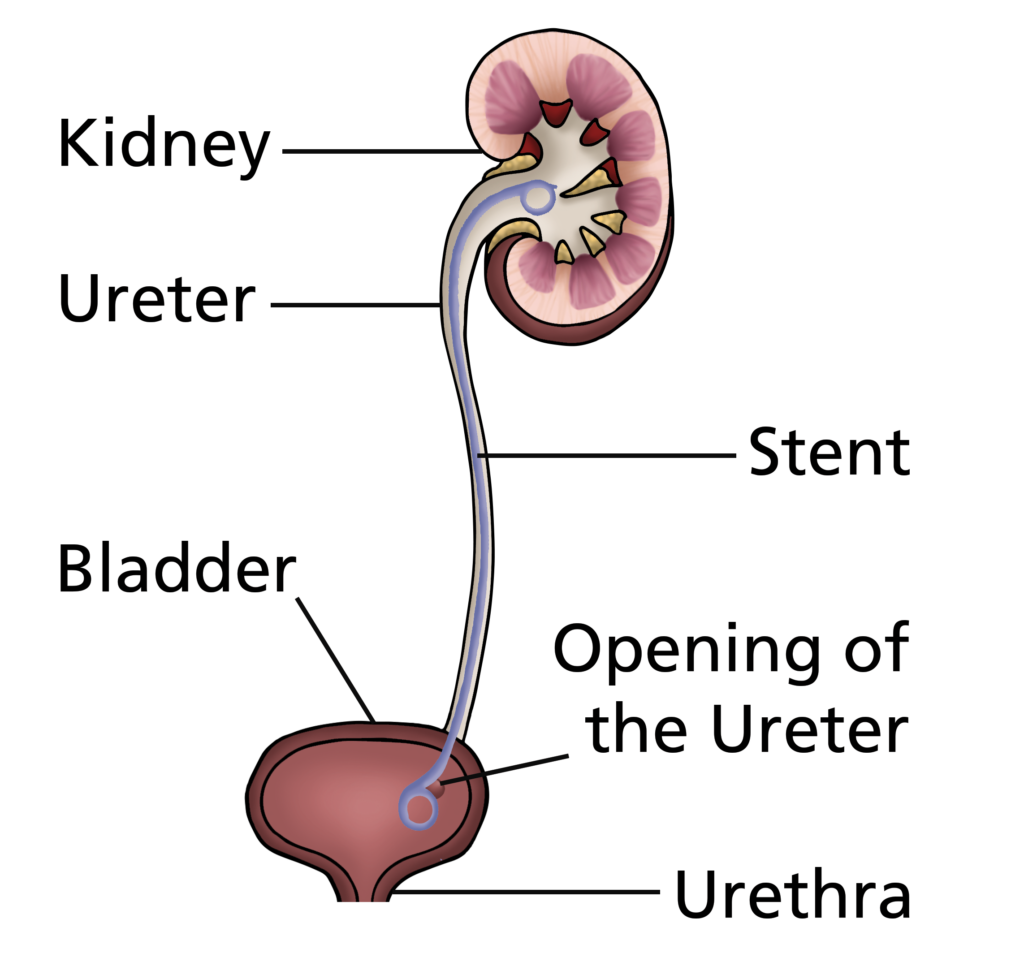
Ureteric stents are inserted for many reasons but the most common indications are blockage of the ureter (the tube draining urine from the kidney to the bladder).
How are stents inserted?
Insertion of a ureteric stent is usually performed under a general anaesthetic. In most cases, in order to insert a stent, the surgeon will need to pass an instrument via the urethra (the water pipe leading to the bladder) and use X-ray control to ensure that the stent is correctly positioned.
The procedure takes approximately 15 minutes to perform and specific consent information is available for this on request.
How long will I remain in hospital?
Your stay in hospital should be no more than one night. Before you go home, you may have an X-ray to ensure that your stent is in the correct position.

What should I expect afterwards?
You may find that, when you first pass urine, it stings or burns and is slightly bloodstained. You may also experience a desire to pass urine frequently and some discomfort in the lower part of your abdomen. Men can experience pain at the tip of the penis and some women develop symptoms similar to those of cystitis. These acute symptoms will, in most cases, settle within 24-48 hours.
Some patients with ureteric stents develop pain in the kidney when they pass urine; this is quite common and is not a cause for concern.
What should I do afterwards?
For the first few days after insertion of a ureteric stent, it is important to drink plenty of fluids, 2-3 litres (4-5 pints) each day, in order to flush your system through. Take regular pain relief.
How long does a stent need to remain in place?
It is usual for a stent to be left in place for anything from two to six weeks although it may remain in place longer during, for example, a prolonged course of lithotripsy.
Ureteric stents are normally removed in the Clinic or in the Day Surgery Unit. You will, of course, be informed of this by letter when you get home.
How is the stent removed?
Stent removal is usually performed under local anaesthetic. A special jelly is used to numb and lubricate the urethra to ensure that the passage of the telescope is as comfortable as possible. The end of the stent is then grasped and the stent removed. If you require a general anaesthetic for stent removal, you will be admitted to the Day Surgery Unit.
Please note that most stents are removed after six weeks or so; if you have not heard about removal of your stent within that period of time, you should let your urology department know to ensure that you have been booked in to have the stent removed.
If you need additional information about the procedure of stent insertion/removal, specific information about consent to these procedures can be provided.
Please ask on the ward or in the outpatient clinic for the appropriate information. This information will become part of the formal process of obtaining written, informed consent for the procedure.
What should I do if no-one contacts me about stent removal?
Most urology departments have a “stent register” to ensure that they do not forget to remove your stent. However, if you have not received any contact within six weeks of your discharge from hospital, please contact the department by telephone.
Are there any other important points?
This publication provides input from specialists, the British Association of Urological Surgeons, the Department of Health and evidence-based sources as a supplement to any advice you may already have been given by your GP. Alternative treatments can be discussed in more detail with your urologist or Specialist Nurse.
Disclaimer
While every effort has been made to ensure the accuracy of the information contained in this publication, no guarantee can be given that all errors and omissions have been excluded. No responsibility for loss occasioned by any person acting or refraining from action as a result of the material in this publication can be accepted by the British Association of Urological Surgeons Limited.
Stent Insertion Record
| Information Provided | Initials |
| By.…………………………………………………………….On …..… /…….. /………. | |
| I understand that I have had a ureteric stent inserted on …..… /…….. /……….as part of my urological treatment. | |
| I have been told that this is a temporary measure and that I might have symptoms that mimic a urinary tract infection (urine frequency, sensation of bladder not emptying fully and blood in my urine). I may also have ache in my loin (where the kidneys are) when I pass urine. If these symptoms get worse, I have been given details about what to do and who to call for further advice. | |
| I have been told that this stent should be removed or changed by …..… /…….. /………. | |
| If the date above passes without a confirmed date to remove or change the stent within a further two weeks, I have been told to contact the Urology/Booking department to ensure the plans for the stent are in place – the key contact details for my surgical team are recorded on the next page. | |
| I have been told that if stents remain in place for more than six months, there is a risk of a urinary tract infection and “encrustation” (where stones form on the coils of the stent, making them more difficult to remove, sometimes requiring further telescopic surgery to remove them). | |
| Name of the surgeon responsible for my care ..………………………………….…………………………… | |
| Name and contact details of the Specialist Nurse for questions about my ureteric stent ..………………………………………………………………. |