This booklet has been produced to provide information for patients undergoing liver resections on the Enhanced Recovery Programme. It is intended to add to the discussions that you will have with your consultant and other team members.
On this page
- Introduction
- The Liver
- Liver Resection
- Enhanced Recovery Programme
- Enhanced Recovery in Liver Surgery (ERAS)
- Before your operation
- Medications
- After your operation
- The recovery period
- Complications that can arise following liver surgery
- Looking after yourself
- Discharge home
- Routine outpatient follow up
- Useful Information
- Contact Numbers
- Useful Contacts
- YouTube video
- ERAS in Liver Surgery at The Leeds HPB & Transplant Centre
Introduction
We realise this is an anxious time for you and your relatives. We hope that by providing accurate information you will know what to expect before and after your operation and hopefully feel better prepared.
St. James’s Hospital is a regional centre for liver surgery, specialising in many different types of liver resection. This is a complex and major operation to remove part of your liver and is carried out for patients who have a tumour in their liver.
These tumours can be either primary cancers, which originate in the liver, secondary cancers which originate elsewhere in the body, or benign lesions in the liver.
The Liver
The liver is the engine house of the body
- It weighs 2% of your total body weight
- You can survive with up to 75% of your liver removed
- After your operation your liver will regrow to the size it needs to function
Liver Resection
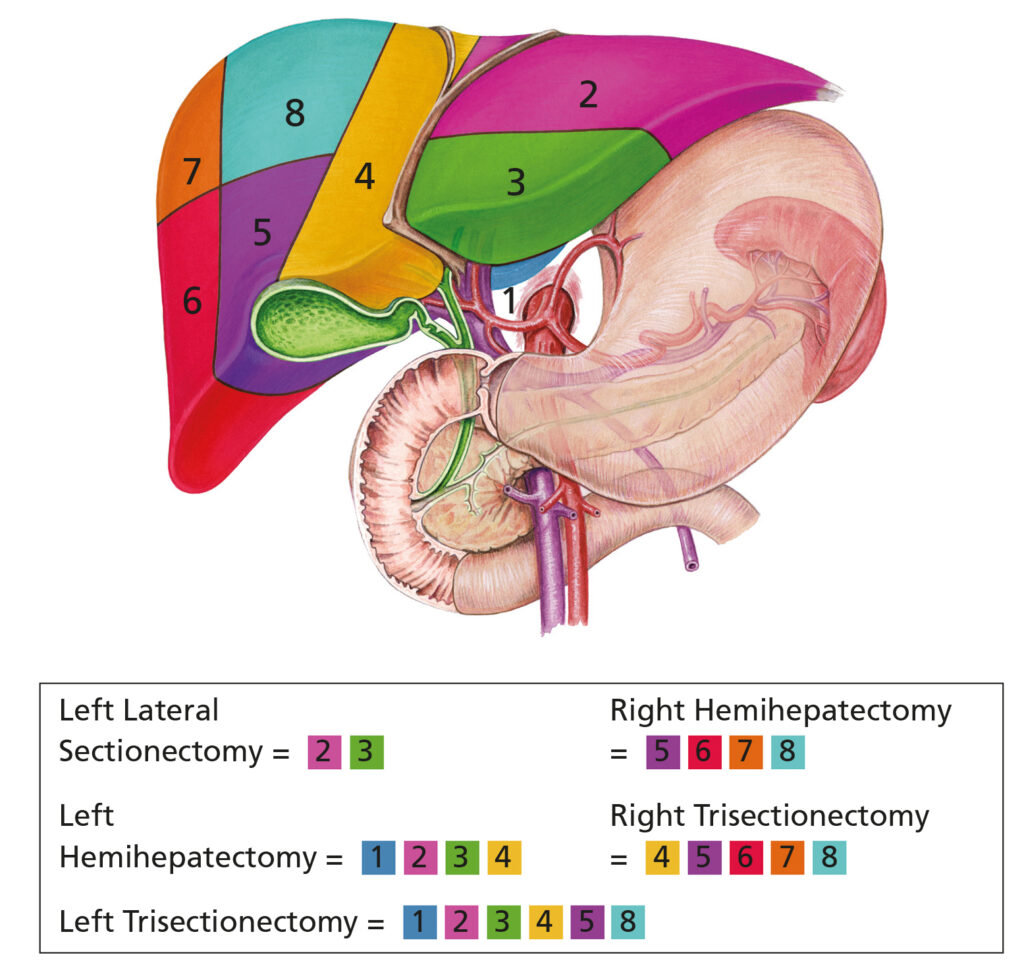
Your consultant will inform you of which resection they intend to perform in your case.
The operation involves removing part of the liver. It may include removing the gallbladder and in some patients the bile duct will need to be reconnected to the intestine.
It is important to remember that very occasionally, at the time of your operation, cancers may be more advanced than previously thought. If this is the case, your consultant may have to carry out more extensive surgery or may not be able to perform the operation.
As with all operations, there is a risk of dying from this surgery. The risk varies with the extent of liver resection, whether your liver is already compromised by pre-existing liver disease, your general fitness and the state of your heart and lungs.
On average 2% of people who have a liver resection will die as a result of having the operation. This means that 98% would survive. Your doctor will discuss this with you in more detail.
Enhanced Recovery Programme
As part of your surgery you will be placed on the Enhanced Recovery Programme. The Enhanced Recovery Programme is about getting you fit before surgery and safely speeding up your recovery time, as well as reducing the incidence of complications. In order for the programme to succeed, you have to actively participate in your own recovery by taking responsibility for certain aspects of your care and recovery.
The main focuses of the programme are:
- Reducing the physical stress of the operation
- Structured approach to post-operative management including pain relief
- Early mobilisation
- Early feeding
- Setting nutritional and daily activity goals
All aspects of this programme will be beneficial to most patients while others may only benefit from certain aspects of it. Depending on your condition of health and fitness at the start, your recovery in this programme may be different from others. Nonetheless, we will try our best to help you use this programme as safely as possible to the best of your ability and needs.
Following major abdominal surgery, patients have traditionally remained in hospital between 1-2 weeks. Recently, it has been shown that by altering how patients are managed both before and after surgery they can be safely discharged home in 5-7 days for open surgery, and 1-3 days for keyhole surgery. We hope that you will achieve this by gaining some control over your recovery.
Enhanced Recovery in Liver Surgery (ERAS)
What you need to start doing
- Diet – increase your protein intake
- Water – aim for 8 glasses a day
- Stop smoking for 4 weeks prior to surgery
- Stop alcohol for 4 weeks prior to surgery
- Exercise – increase your stamina
In the Surgical Outpatients Clinic, you will be given
- ERAS Liver Resection – Information for patients booklet
- Incentive Spirometer – Bring this with you when you come for your operation
- ERAS Liver Video (DVD or YouTube)
After surgery
- Eat and drink as soon as possible
- Aim to walk as soon as possible
- Use chewing gum – to help stimulate your gut
- Learn to self-inject blood thinning injections (this will be explained by ward staff)
Before your operation
Before your operation it is important that you stay as fit and well as you can. Taking regular exercise and eating nutritious food is very important.
If you smoke or consume alcohol, you should try to stop at the earliest opportunity.
Stopping smoking and alcohol, even just a few weeks before your operation, will make a huge difference to your ability to recover from the operation and will also reduce your risk of developing complications.
Pre-Assessment clinic
At the pre-assessment clinic, you will be asked about your general health, previous operations/illnesses, allergies and any medications that you take. You may have an ECG (heart tracing) and/ or chest x-ray as well as some blood tests. If necessary, you may also need to see an anaesthetist.
It is advisable to bring along a relative or close friend to this appointment, who can also be involved and support you with planning your care and recovery. This is an opportunity for you to tell us about your individual needs and circumstances. You should also let us know if any of your circumstances at home change whilst you are in hospital.
Admission to hospital
You will receive a letter through the post with the proposed date of your surgery. The letter will outline the admissions procedure on the day of your operation.
Patients are normally admitted to the Surgical Admissions Lounge. Here you will be asked to change into a warming gown and wear anti-embolism stockings to prevent deep-vein thrombosis (DVT) which are blood clots in your legs.
You will also be asked to wear identity wrist bands and allergy bands if you require them.
Fasting
Fasting means you will not have anything to eat or drink after a specific time.
You should not consume any food from midnight the night before your surgery.
For most patients clear fluids (i.e. water) can be consumed up until 6am the morning of surgery.
Medications
Most medicines should be continued before your operation and throughout your hospital stay; this will ensure you stay in good health. However some of your medicines may need to be stopped before your operation to reduce any risks.
The doctor or anaesthetist will advise you which medicines you should stop and when to stop taking them.
If you have a heart problem, you must take your blood pressure medication, beta-blocker, aspirin and cholesterol lowering medications. If you are taking blood thinning medications such as; warfarin, clopidogrel or tinzaparin / fragmin you must tell the doctor as they will need to be stopped before your operation.
Pain control
Effective pain control is an essential part of the Enhanced Recovery Programme. This will help you to start mobilising, breathe deeply, eat, drink, feel relaxed and sleep well. You will be seen regularly by the acute pain team, who will assess how well your pain is being controlled and try to make you as comfortable as possible. Here are some of the different types of pain relief used post surgery:
Wound catheter and Patient Controlled Analgesia (PCA)
A small ball-like infusion device that delivers continuous pain medications directly into the surgical wound area. This will be placed during your operation. This works alongside a PCA button. You will be given a handset with a button which, when pressed, will give you a controlled dose of pain relief through a line in your arm. For keyhole surgery, patients normally only require a PCA or oral analgesia.
Epidural
This is a small tube in your back which provides a measured and continuous supply of pain relieving medication. This should numb the area over your wound, and will continue for normally 3 days.
After your operation
You will be admitted to HOBs (High Observation Bay) or HDU (High Dependency Unit) following your operation. This will usually be for a day or two for close monitoring. On arrival you will be awake but may feel sleepy. You will have various tubes and monitoring equipment attached to you.
These may include:
Intravenous Fluids
These are given through a line into a vein. This enables the team to make sure your body is getting the right amount of fluids. As soon as you are ready this will be discontinued.
Urinary Catheter
This is a tube that is inserted into your bladder while you are in theatre. It enables us to monitor your urine output to make sure you are well hydrated and your kidneys are working properly. This will be removed once you feel confident mobilising.
Surgical Drain
Often during surgery a drain is inserted into the abdomen to drain away any fluid or blood. This is secured with a small stitch and is usually removed 3-4 days after surgery.
Oxygen Therapy
You will require oxygen for a number of days following surgery. Nursing and physiotherapy staff will encourage you to use an incentive spirometer, which will help to prevent you developing a chest infection.
Incentive spirometer
The Incentive Spirometer will help your lungs fully expand, clear sputum and prevent post-operative lung problems, such as chest infections. You should aim to use it 5 times an hour following surgery.
Place the mouthpiece in your mouth and seal your lips tightly around it. Breathe in and hover the ball in the smiley face (like sucking in through a straw).
Try and hold this for as long as possible. This will allow the white piston to rise and you will hit a target (for example 2000ml). Use the yellow indicator on the right hand side to mark the level you managed to reach.

Aim for this target each time and increase it each day as able. (Wash the mouthpiece with warm water before and after each use)
Circulation exercises
You should also do exercises to help your circulation and reduce the risk of blood clots. Circle your ankles both ways and then point your toes up towards you and then back down briskly. Doing this simple exercise will be beneficial until you are walking regularly.
DVT prevention
After your operation you are commenced on a 28 day course of heparin injections. This helps reduce the risk of blood clots by thinning your blood.
The nurses on the ward will teach you, or someone you live with to self-administer these. Whilst in hospital we encourage you to self-administer the injections with nursing supervision.
The recovery period
The days following your operation will require a lot of effort from you. The nursing and medical teams will encourage and support you. You should aim to sit out of bed each day and gradually increase your mobility and independence. Remember, walking around helps you expand your lungs which helps prevent chest infections. It also helps the blood to circulate which prevents blood clots forming.
What to expect:
| Day 1 after surgery | – Eat and drink as much as able – Assistance with washing and dressing – Pain control device will stay in place – Aim to sit out of bed and walk, with assistance |
| Day 2 after surgery | – Eat and drink as you can manage (1-2L of water) – Become more independent with hygiene needs – Pain control device may be removed and you will be place on regular pain relief tablets – Aim to sit out of bed and walk, with assistance if required – Begin to self administer blood thinning injections with supervision from nursing staff |
| Day 3 onwards | – Eat and drink as you can manage (1-2L of water) – Try become independent with hygiene needs – Continue to take regular pain relief tablets – Sit out of bed for 8 hours, with short rest periods on the bed, and walk around the ward – Continue to self administer injections |
Complications that can arise following liver surgery
As with all major surgery there are sometimes complications involved during and after the operation. Listed below are some complications related to liver surgery:
- Bile Leaks – Within the liver there is a complicated network of bile ducts. It is possible that a small leak can develop. A drain is usually inserted during your operation to drain any excess bile away. A small leak usually heals itself over time and the drain is then removed.
- Fluid Collection – Following your operation a collection of fluid can sometimes develop in the abdomen. This usually re-absorbs and subsides fairly quickly. If the collection persists it is sometimes necessary to have a temporary drain inserted.
- Infection – Any patient undergoing surgery is more at risk of developing an infection. Preventing infection is a high priority for all members of the team looking after you. You will be monitored for any signs of infection and treated appropriately should infection occur.
- Ileus – This is when your bowel stops working following surgery for a number of days. Having an ileus can make you feel sick or you might be sick. We may need to place a tube down your nose and into the stomach to help relieve the distension.
- Bleeding – Some bleeding is expected during the operation and your surgeon can deal with this. Sometimes a blood transfusion is required. If the bleeding continues after your operation, it may be necessary for you to return to theatre.
- Jaundice – Whilst your liver is recovering from surgery, you may develop a yellow tone to your skin and eyes. This may take up to a couple of months to subside until your liver is working normally.
- Encephalopathy – This is caused by a build-up of toxins which are normally cleared by the liver. You may become confused, disorientated or have hallucinations. This is only temporary and usually resolves within 3-5 days following surgery.
- Deep vein thrombosis / pulmonary embolism – Patients having major operations are at an increased risk of developing blood clots in their legs and lungs while they are in bed recovering. These are potential serious complications. You will wear compression stockings, be encouraged to mobilise and have blood thinning injections to help prevent this.
Looking after yourself
- Diet – A varied, high protein diet is recommended to help your body recover. Try eating regular meals, with snacks in between.
- Exercise and activity – Walking is the best exercise during the first six weeks after the operation. Gradually increase the speed and distance you walk. Avoid heavy lifting, strenuous exercise or heavy manual work for the first three months. Do not swim until your wound has fully healed.
- Sex and relationships – You should be able to start experiencing sex as soon as you feel comfortable and are back to your normal levels of activity. For most patients this takes a few weeks.
- Work – You should be able to return to work 4-12 weeks after surgery, depending on your recovery and whether further treatment is required.
- Driving – You should not drive while you are in discomfort. You must speak with your insurance company following any surgery, and be able to safely and comfortably perform an emergency stop before you start driving again.
- Alcohol – You should avoid drinking alcohol for the first 6 weeks following your operation to give your liver a chance to repair itself. You can drink in moderation after this however, we advise that you adhere to the national guideline limits and avoid binge drinking.
Discharge home
When you are ready to be discharged home, the nurses will try and make sure everything is ready for you as soon as possible. Speak to your nurse before arranging a time for someone to pick you up to avoid them having to wait around.
Approximately a week after your discharge, the ERAS nurse specialist will phone you at home to follow up on your progress.
Routine outpatient follow up
You will have an outpatient appointment approximately 4 weeks after your operation – this can be via the telephone or face-to-face. This appointment is to check that you are recovering well and to discuss the histology of the part of the liver removed. It also gives you an opportunity to ask any questions you may have.
For cancerous conditions of the liver, patients are generally followed up with surveillance scans at regular intervals which will be explained by your Consultant. For benign (non-cancerous) liver resections surveillance scans and follow up is not usually required.
Useful Information
Rooms may be available in the Bexley Wing hotel, these can be pre booked once you have confirmation of your operation date. It is free for patients and £35.00 per person per night for relatives or friends. Please be aware rooms are limited.
Contact Numbers
Useful Contacts
YouTube video
Please watch the ‘Enhanced Recovery’ video on YouTube for more information on the programme. Search ‘ERAS Liver Leeds’ or press play below.
ERAS in Liver Surgery at The Leeds HPB & Transplant Centre
Hello, my name is Raj Prasad. I’m one of the liver surgeons here in leads. Welcome to the enhanced recovery program video, which explains to you the principles involved with this program. You might have heard about this program when you were discussing your upcoming liver surgery with your doctors and nurses. Enhanced recovery starts before you come into the hospital when you look at this video and understand the principles and what you are likely to go through when you get admitted at St. James’s University Hospital for your liver surgery.
The main principle of enhanced recovery is you taking control of your own recovery, and uh, this enables you to get better, safer, and quicker than then. What is the normal standard of care? The main principles of enhanced recovery involve mobilising earlier, eating and drinking earlier, and US providing you very good pain relief with newer techniques and technology that allows mobilisation quicker. Over the following segments in the video, you will understand the principles of enhanced recovery in more detail, and I hope you will be able to implement this when you come and get your operation at leads with us. After a decision has been made to go ahead with your operation, we will see you here at the surgical outpatient department.
Here you’ll talk to a surgeon about your options. It’s at this point that we will tell you that you will be placed into the enhanced recovery program. We will also invite you to attend a patient session called the patient recovery education program, or prep. This will be at a later date. If you wish to come to this, we will talk to you about how to prepare yourself before and after your surgery. As part of your treatment, you will be required to attend a pre-op assessment appointment. At the appointment, we will undertake an assessment of your general health and ensure that you are fit for your anaesthetic and procedure. We will also check your blood pressure. Take blood samples and an ECG if it is required, and we will do your MRSA screening. As you’re now part of the enhanced recovery program, we will give you six small bottles of the pre-op drink. We ask that you take four of these bottles the evening before your surgery, and then you will fast on the morning of your operation. We will ask that you take the other two bottles of the pre-op drink.
When you’re admitted into the hospital, please bring with you your overnight things, your medication, and of course the enhanced recovery patient diary on the morning of your surgery. When you arrive in the same day admissions unit, we will ensure that you have fasted the night before and that you have all your pre-up drinks as instructed. A significant part of the enhanced recovery program is warming patients before their operation. One hour before your surgery, you wear a warming gown to make sure that you have the right body temperature and that you feel warm and comfortable. An enhanced recovery program is about employing new techniques in anaesthesia and surgery that promote better outcomes.
There is strong evidence to suggest that patients have few complications and discharge quicker by improving the way we do things. Moving around after your surgery plays an important part in your recovery, and this starts on the first day after your operation if it’s safe, and you feel well enough to do so. Our physiotherapy and nursing staff will help you get out of bed and go for a short walk. Don’t worry about drips and drains; we will help you with them once you are on the ward and able to do so. We will encourage you to walk by yourself regularly. Recording in your diary how far and how often you walk will help you keep track of your progress each day that you’re able to do a little bit more helps to build up the strength to as you were before your surgery. When you have major abdominal surgery, you need to expect to have some pain.
You will either have an epidural wound catheter infusion or a patient-controlled analgesia system during the recovery on the ward. A team of pain specialist nurses will make sure that you get enough pain relief to ensure that you’re able to move around, deep breath, and cough relatively comfortably while recovering on the ward. We will make sure that you continue to do your daily breathing and leg exercises. Using an incentive spirometer as part of your daily routine can help to expand your lung muscles and prevent chest infections. Don’t worry, we’ll show you how to use this. Remember, carry on doing your daily leg exercise. EAS will prevent deep vein thrombosis, or DBT.
We will be there every day to remind you to fill in your diaries and to help get you up and going. On the third or fourth day after your operation, we will start planning for your discharge. We will not discharge you from the hospital unless you are fit to do so and the doctors are happy for you to go. We make sure that you get home as safely as possible. We will also make follow-up phone calls to see how you are coping at home. A big part of the enhanced recovery program is your control over your own recovery. Start calling it my recovery from now on, and if you follow the principles outlined in this video, we can help you get better quicker and safely. For more information about the enhanced recovery program, please get in touch with us.