The treatment is given in the Brachytherapy Department, Rutherford Suite, Level -1 Bexley Wing. Brachytherapy uses a radioactive source held in a small pellet. The source is placed close to the lining of the uterus using special applicators. The treatment area receives a high dose of radiation whilst the dose to surrounding normal tissue is lower. It is given as an alternative to surgery.
The healthcare team looking after you will explain your treatment and the side-effects in detail. If you hear any words or phrases that you do not understand, please ask your doctor or a member of your healthcare team what it means. It does not matter how many times you ask.
Before your treatment
You will be admitted to a ward within the hospital for the duration of you treatment.
You will have a pre-assessment before your treatment start date, this will be an out patient appointment. This is to allow the theatre staff and anaesthetist time to assess you and explain the procedure. The day before your treatment you will be given a small enema to empty your bowels. You will not be allowed anything to eat or drink after midnight.
You will be admitted to a ward on the Monday. The applicators will be inserted on Tuesday morning and your treatment will finish on Thursday afternoon. You will be able to go home later on Thursday or Friday morning.
On the morning of your treatment, you will be helped into a gown and taken to the brachytherapy theatre.
Treatment within the uterus
Two special hollow tubes, called Rotte Y Applicators, are placed inside the uterus. They will stay in place during your treatment (usually three days). During these three days you will have five treatments. This is usually repeated in 6-8 weeks time.
What happens during theatre?
You will be taken to the brachytherapy suite and given a spinal anaesthetic, or in some cases a general anaesthetic is given. This will be decided by the anaesthetist when they discusses your anaesthetic with you. The doctor will insert the applicators into your uterus in theatre. The applicators will be held in position by gauze packing. This may feel uncomfortable but should not be painful.
If you have a spinal anaesthetic you will be awake and be able to feel touching but not pain. You will also have a catheter passed into the bladder so that you do not need to go to the toilet to pass urine.
Next you will be taken for a CT scan to check the position of the applicators and to help us plan your treatment dose.
After the scan, you will be taken back to the ward. You will need to stay in bed, laying flat or slightly propped up, for the next three days whilst the applicators are in place. This is so that the applicators do not move. The nursing staff will help you to wash and make sure you are comfortable. You will be given some tablets to slow down your bowels. You may also have a syringe drive attached to you. This will deliver continuous medication for pain relief and sickness to ensure that you are comfortable.
What happens during treatment?
The brachytherapy treatments are given over three days. The first treatment is on the afternoon that you go to theatre and there will be five treatments in total. The treatments are given in the morning and the afternoon.
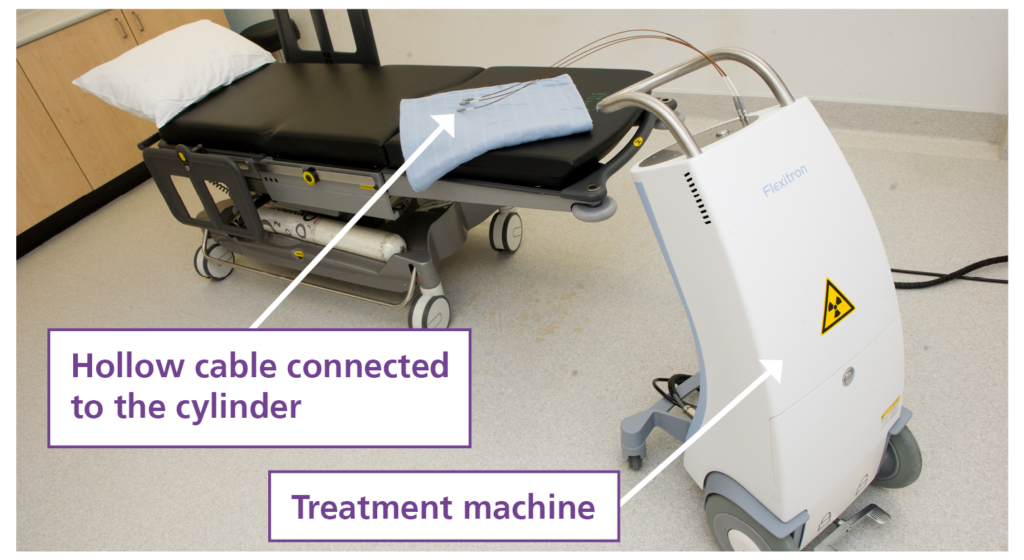
Remaining in your bed, you will be taken from the ward to the brachytherapy suite. When you arrive, the brachytherapy radiographers will connect your applicators to the treatment machine using a series of hollow cables, one for each of the applicators placed in your uterus. The treatment machine (shown below) contains a small radioactive pellet (iridium) which will travel down to each of the applicators in turn.
Whilst the treatment is being given, you will be in the room alone but the brachytherapy radiographers will monitor you using a closed circuit TV. There is also a two-way intercom system so the radiographers can talk to you and you can talk to them. However, please remember to stay still at all times so that your treatment is in the right place.
A radio and CD player can be turned on, if you wish, during the treatment. You are welcome to bring your own music if you prefer.
After each treatment, you will be disconnected from the treatment machine and the brachytherapy radiographers will take you back to your ward
Final treatment
The applicators will be removed by the radiographers after the last treatment.
Once the applicators are removed, you will be taken back to the ward. The catheter will be left in place and be removed by the nurses on the ward once you feel OK.
You can usually go home on the following day
Side-effects
There are a few side-effects related to this treatment.
- Very occasionally the applicators are not in the correct position and will need to be repositioned in theatre or removed. The doctors will explain to you what will happen next if this happens.
- You may feel nauseous while the applicators are in place. This can be treated with anti-sickness medication and should settle when your treatment is finished.
- This treatment can also cause slight bleeding when the applicators are removed.
- You may feel tired. This can continue for some weeks after the treatment.
If these symptoms last for more than 10 days, or start to become more serious after you go home from hospital, you should contact your GP.
When will I see the doctor again?
After the first treatment course you will be given an appointment for the second course of treatment. This will
be approximately six weeks after you have finished your first course.
The doctor will want to see you about 6-8 weeks after all the treatment has finished. An appointment will be posted to you.
Hotel Bexley Wing
The hotel is located on the 8th floor of Bexley wing and offers single and double rooms each with an en-suite, tea and coffee making facilities and digital television. Single rooms with wheelchair access are also available. 23 Patients are able to stay free of charge. There is a charge for relatives if they are staying in their own room. For further details please contact the Hotel Co-ordinator on 0113 206 7687. Out of hours please contact the Non-surgical Oncology Nurse Practitioner through main switch board on 0113 243 3144.
Car Parking Parking for radiotherapy planning and treatment is free. On entering the car park take a ticket and park as usual (disabled parking spaces are on Level 0). When exiting use the left hand lane next to the ticket office. Take your parking ticket and appointment letter to the attendant. They will process your ticket so that when you insert it at the barrier no charge will be made. If you need assistance or are unable to leave your car please press the button on the barrier.
Research at Leeds Cancer Centre
Leeds Cancer Centre is a major centre for cancer research. You may be asked if you would like to help with some of the clinical studies. You are under no obligation to take part in any trials, and your treatment will not be affected in any way if you do not wish to take part.
If you do take part in a clinical trial, you may meet a research nurse or radiographer who will be helping to run the trial
Student radiographers
The radiotherapy department is a training centre for therapeutic radiographers of any gender. They are supervised at all times. If you do not wish students to be present, please speak to a member of staff. This will not affect your treatment or care.
Contact numbers
Brachytherapy Radiographers
Tel: 0113 206 7744 Monday to Friday 8.00am – 6.00pm
Leeds Cancer Support
Complementing care provided by your clinical team, offering access to information and a wide range of support, in a welcoming environment for all. We can be found in the information lounges in Bexley Wing and also in the purpose built Sir Robert Ogden Macmillan Centre.
The Sir Robert Ogden Macmillan Centre
This centre offers a variety of free health & wellbeing and supportive therapies for patients, their family members, and carers. These include hypnotherapy, mindfulness coaching, acupuncture (for hot flushes) and Pilates.
OUTpatients
A cancer support and advocacy charity for the LGBTIQ+ community. Email: [email protected]
Website: https://outpatients.org.uk/
Maggie’s Centre
A warm, welcoming place where you can meet people who are experiencing similar things to you. Next to the multi storey car park. Open Monday to Friday 9.00 am – 5.00pm.
Tel: 0113 457 8364 website: www.maggiescentres.org
Macmillan Cancer Support
Freephone: 0808 808 0000 Open 8am to 8pm seven days a week.
A textphone service for deaf and hard of hearing people is also available. Textphone: 18001 0808 808 0000
website: www.macmillan.org.uk