Your doctor has recommended that you have a Gastroscopy or Colonoscopy. This leaflet will explain the procedure and what to expect on the day of your test.
If you have further questions, please telephone the department or discuss them with a member of the Endoscopy staff before your procedure (please see contact details on pages 7 and 8).
What is a Gastroscopy?
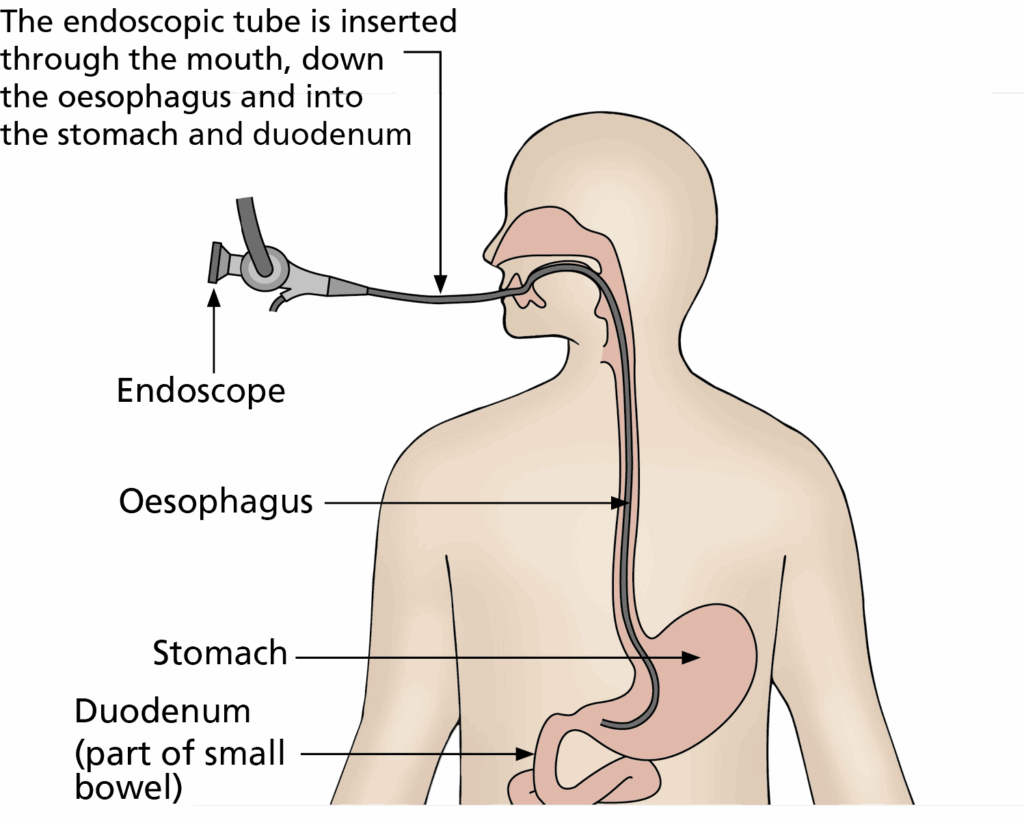
A gastroscopy is a test to examine the upper part of your digestive system – your oesophagus (gullet), stomach and duodenum (small intestine). A flexible tube with a camera on the end is used for this procedure. Pictures from this camera are seen on a television screen by the endoscopist. The test takes between 7 – 15 minutes (depending if treatment is required).
What is a Colonoscopy?
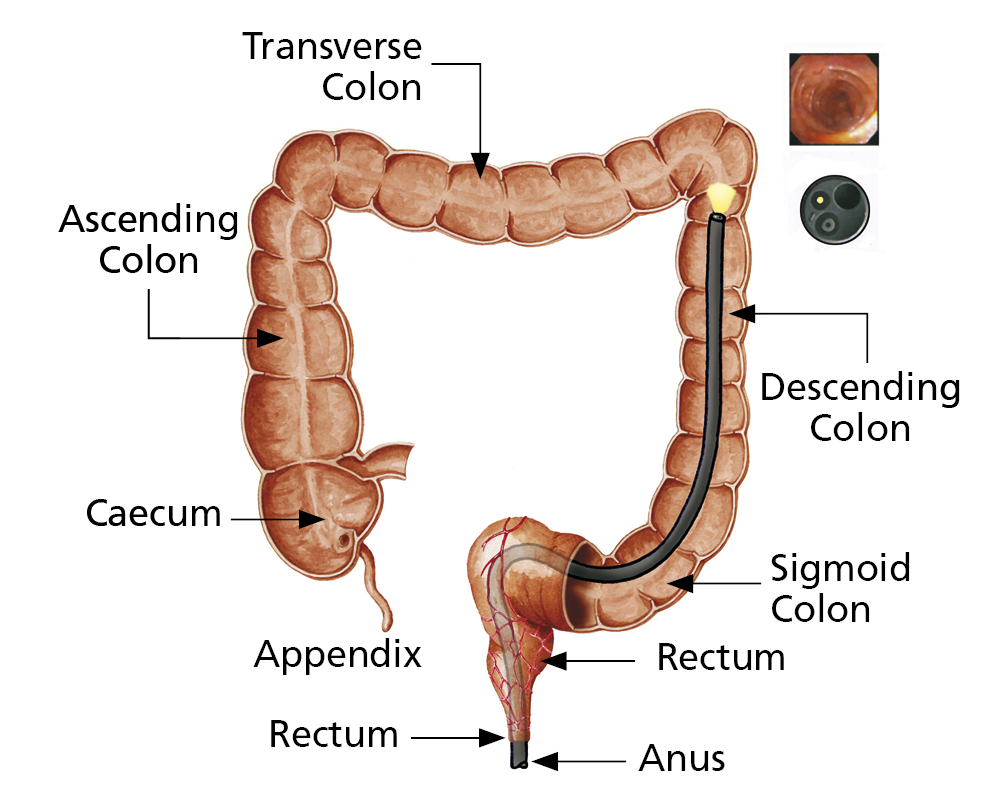
A colonoscopy is an extremely useful test that examines your large bowel (colon). A long, flexible tube with a camera on the end is used for this procedure and is passed through the back passage, and around the whole of your large bowel. Pictures from this camera are seen on a television screen by the endoscopist.
The test takes 30 minutes or more, depending on how difficult it is to pass the camera around the bends in your bowel. To perform both your tests, you should expect to be in the Endoscopy Unit for around 1½ – 4 hours in total.
Why am I having a Gastroscopy and Colonoscopy?
Your doctor has referred you for a gastroscopy and colonoscopy to investigate symptoms you have been having from your digestive system and your bowel such as anaemia, stomach pain, indigestion, diarrhoea, a change in bowel habit or bleeding. Your doctor may want a review of a chronic condition such as colitis or check for recurrence of polyps.
During your gastroscopy and colonoscopy, the endoscopist (doctor or nurse practitioner) may take a small piece of tissue (biopsy) to aid diagnosis. It may also be necessary to remove polyps from the bowel wall. Both removing polyps and taking biopsies is painless, and is achieved by passing special equipment down the inside of the camera. You will not feel this. All tissue samples have to be sent away to the laboratory so the results will not be available straightaway. You will be able to discuss the results of your biopsies with the doctor who referred you.
What are the benefits to having a Gastroscopy
and Colonoscopy?
A gastroscopy and colonoscopy provides detailed information of the appearances of the lining of the digestive system and bowel. The information gained during your test may reveal a cause for your symptoms and will assist your doctor in your further treatment. If you prefer not to have a gastroscopy or colonoscopy, we would advise you to discuss the implications with your doctor.
What are the alternatives to having a Gastroscopy?
There are other methods of examining the stomach such as a barium meal or CT scan. These methods; however, do not allow biopsies and photographs to be taken, and provide less information about the lining of your digestive tract.
What are the alternatives to having a Colonoscopy?
Another method of examining the colon is a CT scan. Although this investigation offers valuable information, it provides less information about the lining of your bowel and does not allow biopsies to be taken, or procedures such as the removal of polyps.
What are the risks of having a Gastroscopy/ Colonoscopy?
The risks associated with your test are detailed on your consent form and below. Please read this. If you have any questions, speak to the nurse or endoscopist on the day, or alternatively, ring the Endoscopy Unit. Complications are rare but it is important that you are aware of them before the test begins. As with any medical procedure, the risk must be compared to the benefit of having the procedure carried out.
What preparation will I need for my Gastroscopy
and Colonoscopy?
For the endoscopist to see the bowel wall clearly, it is essential that the bowel is completely empty. The bowel preparation that has been sent to you works as a powerful laxative and makes your bowel clean. Your bowel preparation medicine and instruction sheet will have been sent to you. Please follow the instruction sheet carefully. It is very important that this preparation works, failure to follow these instructions may result in an unsuccessful procedure. The preparation sheet will also tell you when to stop drinking any fluid. It is important that you stop drinking at the time instructed as gastroscopy must be performed on an empty stomach.
Do I keep taking my tablets?
You must keep taking any essential tablets unless your doctor tells you specifically not to. Please take you tablets early morning with a sip of water.
- If you are taking iron tablets (ferrous sulphate), please stop them seven days before your test.
- If you are taking Codeine, Loperamide (Immodium) or
Co-phenotrope (Lomotil), please stop three days before the start of your procedure. - Please telephone the Endoscopy Unit if you are diabetic, have sleep apnoea or are taking tablets that prevent blood clots. Examples of blood thinning tablets are Warfarin, Dabigatran, Apixaban, Rivaroxaban, Edoxaban, Aspirin, Clopidogrel (Plavix), Dipyridamole (Persantin), Prasugrel (Efient), Ticagrelor (Brilligue) or Acenocoumarol (Sinthrome).
- Women taking the oral contraceptive pill should be aware that taking bowel preparation might prevent the absorption of the pill. Additional contraceptive precautions should be taken until the next menstrual period begins.
What should I bring on the day?
Please bring a list of medication that you take and also any medication that you may require, whilst in the department such as GTN spray, inhalers and insulin. Please do not bring any valuables to the department or wear lots of jewellery. Please can you also ensure that you remove nail varnish as this interferes with the signal we receive from our monitors about your oxygen levels.
You may wish to bring your dressing gown and slippers. You will be asked to change into a hospital gown that is open at the back, before your test.
Choosing how to have the test – what is the difference between throat spray, sedation and Entonox?
You will need to decide if you want to have throat spray or sedation for your gastroscopy, or Entonox or sedation for your colonoscopy. If you have throat spray for your gastroscopy and Entonox for your colonoscopy, you will be able to leave the department around 30 minutes after the procedure is complete, if you are feeling well and the recovery nurse has no concerns.
If you decide to have sedation for your gastroscopy, this will keep you comfortable during your colonoscopy procedure also. Please read the information below regarding the sedation as this affects the time that you will be in the department, and also, the aftercare that you will need to arrange before you come for your test. Both procedures will take around 60 minutes to complete.
On the day of your procedure, or during your pre-assessment appointment, the options will be discussed with you. Please note that all patients requesting sedation will be assessed to determine if they are medically fit for the administration of sedation.
During gastroscopy, many patients are concerned at the thought of swallowing the tube but we would reassure you that the test is not painful, you will be able to breathe normally and you will not choke. This is because the camera is in your food pipe and this is seperate to your breathing pipe. During the test, we have to inflate your stomach with air, some patients find this unpleasant.
Please note:
Although, the choice of sedation / throat spray / entonox is yours to make, the endoscopist / admission nurse may advise you on the option that may be more appropriate considering your medical history (see risks associated with sedation).
What will happen on the day of the test?
When you arrive at reception in the Endoscopy Unit, your personal details will be checked. The assessment nurse will collect you and take your medical history, discuss your choice of pain relief, explain the test and take your blood pressure and pulse. You will be able to ask any questions and discuss any worries or questions that you have about the test. You will be asked for your consent form (supplied with this leaflet). This will be attached to your notes and taken to the procedure room.
Please make sure that you have read the consent form through before you come for your test as when you sign this form you are agreeing that this is a test you want. Remember, you can change your mind about having this procedure at any time. The endoscopist will discuss the consent form with you.
Please note:
Every effort will be made to see you at your appointment time; however, unexpected delays may occur. The endoscopy staff will keep you informed of any delays in the department.
What happens in the procedure room?
You will be greeted by two nurses who will remain with you during the test. The nurses and the endoscopist will complete a checklist to ensure that all your information is correct. If you have chosen to have sedation, a cannula will be placed in your vein so that sedation can be administered and you will be given oxygen through a small plastic tube in your nose. If you are having throat spray, your throat will be numbed.
You will then be asked to remove any dentures or glasses and lay on a trolley on your left-hand side. All patients pulse and oxygen levels are monitored by a probe placed on your finger during the test. Before the test starts, a plastic mouthpiece is placed between your teeth to keep your mouth slightly open.
When the endoscopist gently passes the endoscope through your mouth, you may gag slightly – this is quite normal and will not interfere with your breathing. During the procedure, air is put into your stomach so that the endoscopist can have a clear view. This may make you burp a little, some people find this uncomfortable.
Most of the air is removed at the end of the test. When the procedure is finished, the endoscope is removed quickly and easily. If you become uncomfortable or want the procedure to stop at any point, you can indicate this by raising your hand.
After your gastroscopy is completed, the endoscopist will then begin your colonoscopy. If you are having Entonox, the nurses will show you how to use the mouthpiece that delivers the gas. The endoscopist will initially examine your back passage with a finger to make sure it is safe to pass the camera and then introduce the colonoscope into your back passage and guide it around your bowel.
During the procedure, the endoscopist introduces air into the bowel. You may experience bloating from the air and cramp like pain as the camera goes around bends of the bowel. Air can be relieved by passing wind (this is normal and you must not be embarrassed as the endoscopist will expect you to do this). If you are finding the procedure more uncomfortable than you would like, please let the nurse know and you may be given more sedation or a painkiller.
You may also be asked to change position during the test
e.g. roll onto your back to make the procedure easier and more comfortable. If the test continues to be uncomfortable, a decision may be made to end the test. A colonoscopy usually takes 30 minutes but can differ, depending on how difficult it is to pass the camera around the bends of your bowel.
Please note:
All hospitals in the trust are teaching hospitals and it may be that a trainee endoscopist performs your procedure under the direct supervision of a consultant, registrar or nurse practitioner.
What happens after the test?
You will be transferred to the recovery room after the test. The length of your stay is dependant on if you have had sedation or throat spray / Entonox.
If you had local anaesthetic spray and Entonox for your test, you can leave the department after the recovery nurse has checked your blood pressure. If you feel well, you will have to wait 1 hour before you have anything to eat or drink as the throat spray can make swallowing difficult.
If you have had sedation, the recovery nurse will monitor you during your recovery from sedation. This can take 2 – 3 hours.
Remember: if you have sedation, you will need an escort with you, some transport home and someone to look after you for 24 hours after the test.
You must not
- drive a vehicle;
- drink alcohol;
- operate machinery (applies to sedated patients only);
- go to work (applies to sedated patients only); and
- sign legal documents.
The recovery nurse will prepare you for discharge home and give you after-care instructions. You may experience a sore throat, feel bloated and experience some stomach cramps due to the air left in your stomach and bowel. Both sensations are normal and should clear up quickly.
When will I get my results?
A full report will be sent to your referring doctor and your GP. The endoscopist or nursing staff will usually have the opportunity to speak to you after your test regarding the results. Some patients will receive their test results via letter, or if appropriate, some may receive a clinic appointment through the post. Any enquires regarding your outpatient appointment should be directed to your consultant’s secretary. If you feel that you are waiting a long time for an appointment to discuss your results, your GP will also have a report so you can see them too.
This leaflet has been designed as a general guide to your test. If after reading this, you have any questions that you feel have not been answered, please contact the Endoscopy department on the numbers below.