This booklet explains what fibroids are and the options available for their treatment. Please speak to your doctor if you require more information about any of these treatments.
What are Fibroids?
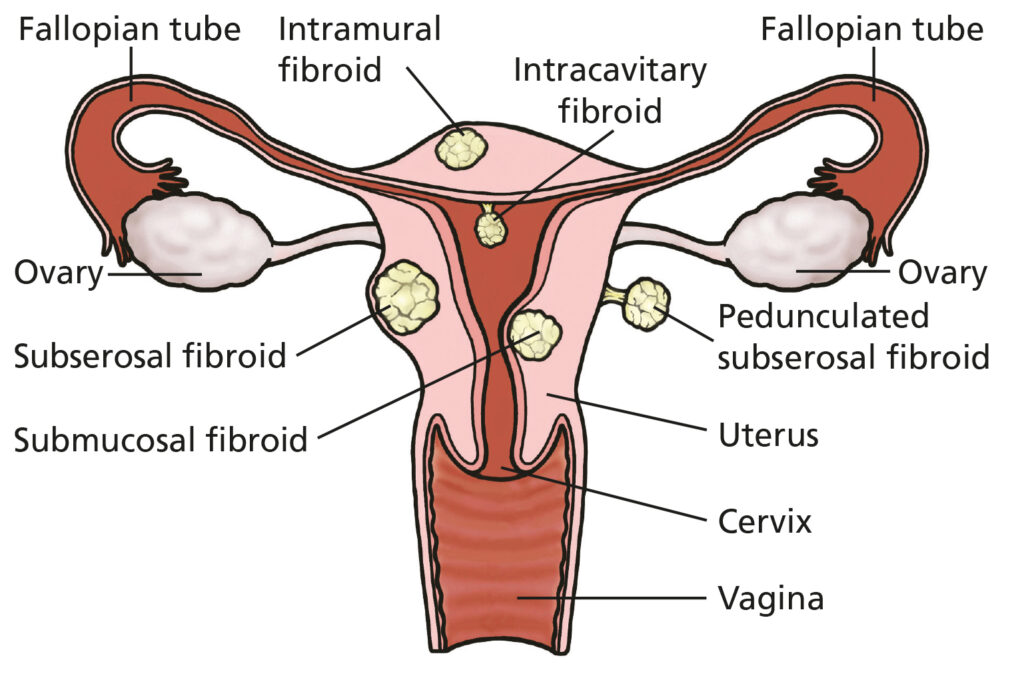
Fibroids (medically known as leiomyomas) are common, non-cancerous growths that develop from the muscle of the womb. Fibroids are made up of both muscle and fibrous tissue and may vary in size and position within the womb.
Fibroids are very common. 20-50% of 30+ year olds may have at least one fibroid. Fibroids do not always cause problems and many women may never know they have them. They are rare in teenagers and shrink after the menopause (when the periods stop for good). Fibroids may be often found by chance when other symptoms are being investigated. Sometimes fibroids do cause symptoms which can vary in nature and severity depending on their size and position.
Some symptoms associated with fibroids are:
- Heavy periods.
- Painful periods.
- Tummy or lower back pain.
- Pressure symptoms on your bladder or bowel making you feel that you need to go to the toilet often.
- Constipation.
- Pain or discomfort during sex.
- Difficulty in getting pregnant.
- Miscarriages.
- Iron deficiency anaemia.
Advice for all women with fibroid
Large fibroids, or those that are mostly on the outer surface of the womb (subserous fibroids) are more likely to cause pressure symptoms. Fibroids that mostly face inwards (submucous) are more likely to cause heavy periods and may cause fertility problems.
Fibroids can also be associated with risks in pregnancy including miscarriage, premature labour and an increased risk of a Caesarean section delivery due to the baby lying in an unconventional position e.g. bottom first or obliquely. There is also a higher risk of heavy bleeding during pregnancy and after the baby has delivered. Fibroids can affect you in different ways, and the treatments offered to you will depend upon the type of fibroids you have and your symptoms and also taking into account you as an individual including your age and whether you are planning a pregnancy. You will have a personalised plan discussed with your specialist.
If you notice any changes in your bleeding pattern, you feel your abdomen is swelling, you experience bladder or bowel pressure symptoms (for example frequently needing to empty your bladder or difficulty opening your bowels), or if you feel that your treatment is not working, then please contact your doctor for a review.
Medical treatments for fibroids
These are usually recommended:
- If your symptoms are mild.
- If surgery is not safe enough or appropriate for you.
- If you are approaching your menopause when your periods will stop and the fibroids will shrink.
- To improve your iron levels (reduce anaemia) and make your operation safer.
Mefenamic acid and tranexamic acid
Mefenamic acid tablets can provide pain relief due to cramps and tranexamic acid tablets help to reduce the blood loss. They need to be taken with each monthly bleed.
Hormonal medication
These methods are not suitable if you are actively trying to get pregnant, but can be used temporarily while planning fertility treatments or before surgery.
Combined oral contraceptive pill
This pill acts on the lining of the womb and may help to reduce the heavy bleeding that fibroids can cause, and may also prevent the fibroids you have getting bigger.
Progestogens
Progestogens are synthetic versions of the hormone progesterone and can help by reducing menstrual blood loss, preventing the fibroids from getting bigger as well as helping them to shrink. Progestogens can be taken in the form of an oral pill or an intrauterine coil system called the Mirena.
GnRH analogues
This medication brings on a temporary menopause which can help to shrink the size of the fibroids and stop the periods. This medication is also sometimes prescribed before myomectomy surgery to reduce the blood loss during the operation. GnRH analogues can produce side-effects such as hot flushes, difficulty sleeping, dryness in the vaginal area, and also bone loss (early osteoporosis). Taking GnRH analogues for more than six months can lead to thinning of the bones (osteoporosis) unless some oestrogen hormone is taken to balance this together with progesterone (Hormone Replacement Therapy (HRT)). It is possible to do this for up to two years before taking a break and checking bone strength with a bone (DEXA) scan.
Ryeqo®
Ryeqo is a new daily tablet treatment for moderate to severe fibroids which works in a similar way to GnRH analogues above but is reported to have fewer side-effects. About 3/4 of women taking it found their blood loss to reduce by about half.
Other non-surgical treatment
Uterine artery embolization (UAE)
This is a procedure done in the x-ray department where small gel-like particles are guided into the main feeding blood vessels of a fibroid through a catheter tube inserted into a blood vessel in your groin (under local anaesthetic). This stops the blood supply to the fibroid causing it to shrink and break down.
It is a relatively new technique and the outcomes are still being monitored. Nine out of 10 people treated in this way are happy with the outcome (reduction in heavy bleeding).
The advantage of UAE is a shorter hospital stay and a quicker return to routine activities.
There is a risk of cutting off the blood supply to a larger portion of the womb which could make it harder or impossible for a pregnancy to attach properly and grow normally.
There is also a risk that the gel particles could reach the artery to the ovary and affect the egg supply (risking early menopause or infertility). Successful pregnancy after UAE is certainly possible and has been frequently reported in the scientific journals.
Generally speaking, it is not recommended if you are still trying to have children. More detailed information is available separately on UAE. Please ask if you are interested and have not been offered it.
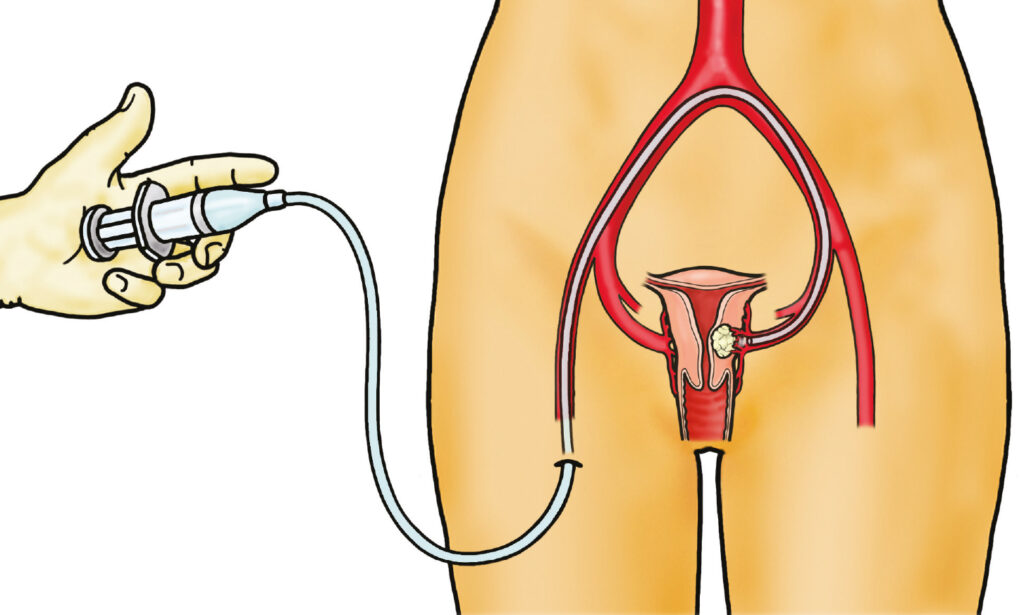
UAE is done by putting a catheter into the big artery in the groin under local anaesthetic. The catheter is fed up the vessel and into the artery supplying the womb and branches leading to the fibroid. Tiny beads are then injected which block the artery and ‘cut off’ the fibroid.
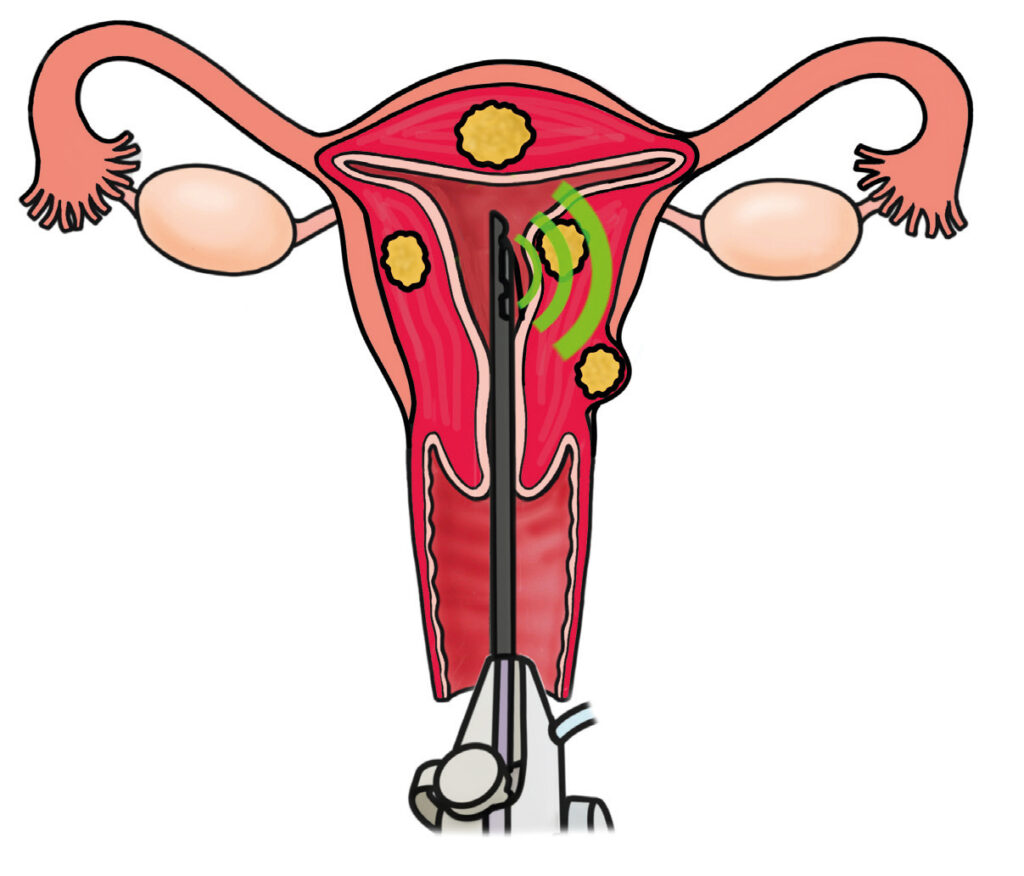
SONATA
Sonata radiofrequency ablation is usually an outpatient procedure. It can provide safe and effective treatment of fibroids that cause symptoms. There may be some fibroids not suitable for Sonata due to their size and location.
It is not currently offered to women wishing to fall pregnant in the future although there have been cases of healthy pregnancies after Sonata.
- Under local anaesthetic, your clinician passes the Sonata treatment hand piece into the vagina and through the cervix to enter your womb (like a keyhole instrument).
The hand held device
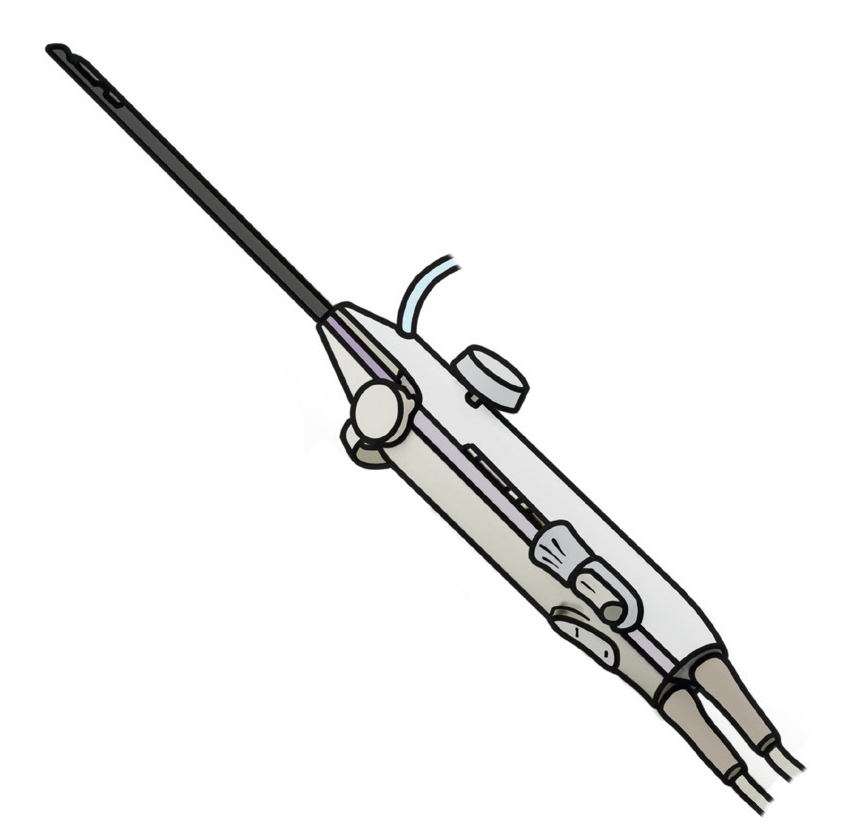
- Ultrasound waves from the tip of the device are used to locate the fibroid (s).
- The Sonata treatment handpiece delivers radio frequency heat into the fibroid which then shrinks over time and reduces symptoms.
- Please ask for a leaflet for more written information.
Surgical treatments for fibroids
What is a myomectomy?
A myomectomy is an operation to remove fibroids, whilst retaining the womb, fallopian tubes and ovaries. Whether a myomectomy is the best choice or not for you depends upon your age, the need to preserve fertility, the size, number and positions of your fibroids.
Myomectomy is mostly recommended if you wish to retain your fertility.. The other surgical option for management of fibroids is a hysterectomy, which involves removal of the womb and all the fibroids in it.
What does the myomectomy procedure involve?
A myomectomy operation can be done either by approaching the fibroid through the surface of the womb (by Laparoscopy/ key-hole surgery or Laparotomy / an open cut) or through the cavity of the womb (by hysteroscopy / key-hole surgery through the vagina).
Laparotomy i.e. ‘open’ surgery
This is the most traditional way of performing a myomectomy. The operation is done through either a bikini line cut, or an up-and-down cut on your tummy. This will depend on the size of the fibroid(s) and whether you have had any previous operations.
Laparoscopy i.e. ‘keyhole’ surgery
This procedure is performed by introducing a telescope through the belly button and miniature instruments through other small incisions in the tummy. This approach may not be suitable for you but your surgeon may offer this option if it is a possible in your case.
Robot assisted Myomectomy?
Robotic-assisted surgery involves the surgeon operating using a console that control instruments within your body.
The procedure is in 3D and additional range of motion of the instruments can improve surgical precision and control. Your surgeon may feel that you might benefit from a Robotic approach to your myomectomy and offer this to you.
Hysteroscopy
This is the preferred approach if the fibroid is mainly occupying the cavity of the womb. The procedure can be performed under general anaesthetic (more traditional), or under local anaesthetic (special fine telescope device) in the outpatient hysteroscopy department. This will depend on the size of the fibroid, availability of facilities and your wishes.
How long will I be in the hospital?
- Following a laparotomy, you will need to stay in the hospital for 2-5 days. You will have a urinary catheter (small plastic tube to drain the bladder) after the procedure for about 1-2 days.
- After a key-hole operation you may be discharged home the same day or may need to stay in hospital for 1-2 days.
What is the recovery time?
This depends on the surgical approach. Typical recovery times are:
- 4-8 weeks after laparotomy.
- 2-3 weeks after laparoscopy.
- 2-3 days after hysteroscopy.
When will I be able to try to get pregnant?
The womb must be allowed to heal from the removal of a fibroid / fibroids. Pregnancy will put the scar(s) under strain and they need to be allowed to strengthen beforehand.
You are advised to avoid pregnancy for 3 months after your operation to reduce the risk of the scar(s) tearing which may be dangerous for you and your baby.
What are the risks associated with a myomectomy?
Bleeding and blood transfusion
The risk of very heavy bleeding is very low. Bleeding can usually be managed with keyhole surgery techniques but rarely (less than 1 in 100 operations) the operation needs to be extended into a larger incision called a laparotomy to be able to stop the bleeding from becoming dangerous. The transfusion of blood is not commonly needed but it will be done if necessary to top up heavy blood loss.
Infection
Infection does sometimes happen in the skin wounds as they are trying to heal afterwards. It is important to keep the wounds clean and follow your aftercare instructions.
Damage to nearby structures
The pelvic organs (bladder, womb, tubes, ovaries and intestines) are all close to each other in the surgical area. The ureter is the tube that connects the kidneys to the bladder. This tube is also in the area, close to the blood vessels going to and from the legs. All these structures are vulnerable to damage as a result of surgery close to them. These complications are not common but they can be serious if they do occur.
Damage to the bowel (small pin-prick or tear) can lead to infection as the contents leak out. The chance of this complication is lower than 1 in 2000 operations. Sometimes it is obvious and can be fixed at the time but sometimes it is hidden and does not cause problems until a couple of days after the surgery. If you do not feel much better or if you have pain and a temperature (sweats and shivers) by the third day after your operation you should contact the ward and attend for a check-up.
Blood clots (deep vein thrombosis, pulmonary embolus)
Blood clots in the deep veins of the legs can happen when you are lying or sitting still for a long time. If you smoke and / or are overweight and / or are taking oestrogen hormones you are more at risk.
We recommend you wear compression stockings during your admission and will be encouraged to get up and get moving soon afterwards to keep the blood in your legs flowing.
You should continue to get up and about at home as well. Hydration is important and you should keep drinking plenty of water even if you do not feel like eating much in the day or so after your operation. Some people judged to be at increased risk will be given blood-thinning injections as well.
General anaesthetic
The risk of serious problems with general anaesthetics is lower if you are younger. Allergic reactions are rare and can be managed. You should discuss any particular concerns you have when the anaesthetist visits you before the operation to explain what they will be doing for you to keep you comfortable during and after the procedure.
For myomectomy specifically
Scarring in the womb cavity
The risk is higher with hysteroscopic fibroid removal (from the inside) or if the cavity of the womb is opened during a laparoscopy or laparotomy approach. This is more likely with large fibroids stretching the full thickness of the womb muscle wall.
Hysterectomy
It is very unlikely (less than 1% of all myomectomy operations) that a hysterectomy (removal of the womb) will be required but it does sometimes need to be done as it may be the only way to stop very heavy and life-threatening bleeding.
Recurrence of fibroids
There is a risk of new fibroids growing within five years of surgery. This risk is very difficult to predict, but is higher is higher if you are younger or you are of afro-Caribbean ethnicity.
Caeserean delivery
If your fibroid is large enough to span from the inside (cavity) to the outer surface of the womb, or if the cavity of the womb is opened during the operation, this may weaken the wall of the womb increasing the risk of rupture during labour. You may therefore be advised to have a planned Caesarean birth..
What is a hysterectomy?
This is the complete removal of the womb. The ovaries may be left in place and can continue to work (produce hormones) until the menopause occurs. A hysterectomy may be recommended if you have completed your family and no longer wish to get pregnant, especially if your fibroids are large and you wish a permanent solution to your symptoms.
A Hysterectomy is guaranteed to stop period bleeding and is a good way of relieving pressure off the bladder. There are risks and side-effects that should be discussed carefully with your doctor.
Myomectomy and hysterectomy compared
| Abdominal myomectomy | Hysterectomy |
| Pregnancy: may be possible afterwards although this depends on many other factors as well. Aims to preserve the healthy womb tissue. | Pregnancy: not possible afterwards. Removes the womb with or without the neck of womb (cervix) = total / subtotal hysterectomy. |
| Not usually offered if another pregnancy is not planned: consider hysterectomy if other treatments have not been good enough. | |
| Incision: bikini line or vertical, depending on the size of the fibroids | Incisions: bikini, vertical, keyhole, vaginal. Your surgeon will advise the most likely but sometimes the final decision is not made until the operation has begun. Smaller incisions usually mean a shorter recovery time. |
| Periods will continue and should be improved (lighter flow, possibly less pain). | Periods will stop for good. |
| The removal of the Fallopian tubes and ovaries may be discussed which can reduce the risk of ovarian cancer in the future (the background risk of developing ovarian cancer is 2 women in 100 but this risk is higher if you carry the BRCA gene mutations. Your doctor will discuss your specific risk if necessary). IMPORTANT NOTE: If you are having a hysterectomy as treatment for fibroids you will most likely not have your ovaries removed. |
Both operations have similar:
- Risks (blood loss, pain, infection, blood clots or thrombosis),
- Length of time in hospital (2-4 days)
- Recovery times (4-6 weeks)
when done through a tummy cut.
Glossary
- Anaemia: This is a condition where there are not enough red blood cells to meet the body’s needs. This causes tiredness and weakness and when it is extreme, dizziness or fainting.
- Embolization: The active blockage of a blood vessel to starve the tissue downstream. Sometimes this can be therapeutic e.g blocking the uterine artery branches to large fibroids to make them shrink. Sometimes it can happen naturally as part of an illness and be very serious e.g. some strokes are due to embolization of naturally-formed clots which block the blood supply to part of the brain.
- GnRH: Gonadotrophin releasing hormone: This hormone is released by the brain as part of the reproductive hormone cycle. Medicines exist to block it which prevents the menstrual cycle from happening (stops the periods).
- Menopause: When the monthly periods naturally stop because the ovaries are no longer producing eggs and hormones. The common time for this to happen is 51 years of age.
- Miscarriage: Any positive pregnancy test which does not reach 24 weeks of pregnancy.
- Progesterone / progestogen: The hormone (natural / synthetic) that is produced in the second half of the menstrual cycle (by the ovary) to prepare the womb lining for pregnancy. Large amounts of progesterone are produced in pregnancy. Synthetic progesterone (progestogen) is often used in hormonal treatments for bleeding problems and contraception.