On this page
- What is a high output stoma or fistula?
- Why might I have a high output?
- Anatomy of the digestive system
- Eating and drinking with a stoma or fistula
- Reducing the fibre in your diet
- What can I eat
- What about vitamins and minerals?
- Dioralyte®
- St Mark’s electrolyte mix
- Which medications might help to reduce my stoma or fistula output?
- What should I do if I am losing weight?
- Useful contacts:
This following information provides advice for patients and/or carers of patients who have a high output stoma or fistula. It provides information on what to eat and drink, and medications to help manage symptoms.
What is a high output stoma or fistula?
A stoma is when part of the bowel is brought out onto the surface of the skin. For example, a jejunostomy, an ileostomy or a colostomy.
A fistula is a connection between the bowel and the skin that can develop for a variety of reasons.
A high output stoma or fistula is when you have high losses over an extended period of time. This means you are emptying your stoma bag many times each day and the content is watery. The output from the stoma or fistula varies from patient to patient, so there is no set amount that can be defined as high output.
Back to topWhy might I have a high output?
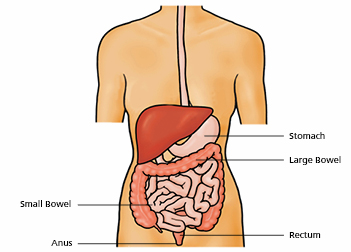
To help understand this, it is helpful to know what usually happens when someone eats and drinks:
- Stage 1 – Food is chewed in the mouth and swallowed.
- Stage 2 – The food passes down the food pipe (oesophagus) into the stomach.
- Stage 3 – In the stomach food is churned and mixed with acid.
- Stage 4 – The mixture passes into the small bowel
- where it is digested. This is where the nutrients are
- absorbed.
- Stage 5 – Any bulk remaining then passes into the large bowel (colon). This is where water and salt are taken back into the bloodstream which helps to make a formed bowel motion.
- Stage 6 – The bowel motion is stored in the rectum until it is ready to be passed.
- Stage 7 – The bowel motion is then passed out through the anus as faeces (stool) when you go to the toilet.
Anatomy of the digestive system
Eating and drinking with a stoma or fistula
When you have a stoma or fistula, you will not go through all these stages. The site of your stoma or fistula within your digestive system will affect which stages are missed. Part of stage 4 and stages 5 – 7 may no longer occur. This means that fluids and nutrients move through too quickly for the remaining bowel to absorb what it needs. Depending on your medical history, the remaining bowel may also struggle to absorb enough fluid and nutrients.
Back to topReducing the fibre in your diet
Reducing the amount of fibre in your diet can help reduce your stoma or fistula output and help you absorb more fluid and nutrients. You should base your diet around the Eatwell guide, but should try to avoid foods high in fibre as shown in the following table:
| Foods to avoid | Foods to choose | Foods to avoid |
| Bread, rice potatoes, pasta and other starchy foods | White bread and rolls. Foods made with white flour e.g. chapattis, pitta, muffins and crumpets White pasta or rice Couscous Plain crackers, rice cakes and crispbreads Cornflakes, Rice Krispies, Special K, Coco Pops, Frosties and porridge oats (thin consistency) Potatoes without skins | Wholemeal, wholegrain or multi seeded bread and rolls Wholemeal pasta, brown and wild rice Wholegrain and rye crackers Wholegrain breakfast cereals or those containing bran, fruit or nuts e.g. All Bran, Fruit and Fibre, Weetabix, and muesli. Wholegrain cereal bars Potatoes with skins/jackets |
| Milk and dairy foods | Milk and milkshakes made with flavoured syrup Plain milk puddings e.g. tapioca, rice pudding and custard Plain or smooth fruit yogurt or fromage frais Plain hard or soft cheese. Cottage cheese and cheese spread Ice cream | Milk puddings with nuts or dried fruit Yogurt or fromage frais containing fruit pieces, nuts or seeds Cheese with added fruit or nuts Ice cream with fruit pieces e.g. Rum and Raisin |
| Foods and drinks high in fat and/or sugar | Plain white, milk or dark chocolate Boiled or jelly sweets, brown or white sugar, syrup, seedless jam and honey and sugary drinks Plain cakes or biscuits e.g. Victoria sponge, shortbread, Rich Tea or Nice Oil, butter, margarine, dressings, mayonnaise and salad cream Smooth peanut butter | Chocolate and sweets with fruit or nuts Marmalade with peel or Jam containing seeds or pips Cakes or biscuits with dried fruit or nuts, malt loaf, wholemeal biscuits e.g. Digestives or Hobnobs Crunchy peanut butter |
| Meat, fish, eggs, beans and other non-dairy sources of protein | Soft, tender, well cooked meat or fish Boiled, poached or fried eggs Tofu | Meat or fish in sauce that contains vegetables or beans Tough or fibrous meat or gristle Quorn All beans and pulses e.g. lentils, kidney beans, chickpeas All nuts and seeds |
What can I eat
Eatwell guide 2016 FINAL MAR29
Fruit and vegetables
Fruit and vegetables are generally high in fibre. Reducing the amount of fibre you eat can help reduce your stoma or fistula output.
It is recommended that you try to avoid:
- Raw salad vegetables e.g. lettuce, tomato, cucumber
- Stringy fruit and vegetables e.g. celery, green beans, pineapple
- Seeds and pips e.g. berry fruits, kiwi fruit
- Skins/peel and shells e.g. apple, pear, peas, sweetcorn
- Dried fruits
Some fruit and vegetables can be included in small amounts:
- Melon
- Peeled, tinned/stewed fruit
- Passata
- Peeled, well-cooked root vegetables e.g. turnip, swede, parsnip, carrot
- Ripe banana
If you are an inpatient, you may also find it useful to refer to: A Guide to Choosing a Low Fibre Diet from the Hospital Menu. Your dietitian can provide you with a copy of this.
Other tips
- Eat slowly and chew your food well. This will help your body to digest food
- Add extra salt to your meals
- Choose salty foods and snacks e.g. bacon, ham, sausages, tinned food in brine, Marmite or Vegemite, salted crisps and biscuits
- Avoid heavily spiced foods
What about vitamins and minerals?
- If you have had a high output stoma or fistula for some time, you may have become deficient in vitamins and minerals, commonly magnesium. Your team may prescribe a supplement to help replace these losses
- If you have had the last part of your small intestine removed, you will need to have regular vitamin B12 injections. Ask your team if you will need these.
Dehydration
When you have a high output stoma or fistula you may become dehydrated quickly. It is very important that you learn to recognise the signs of dehydration.
Symptoms of dehydration can include:
- Cramps
- Dark sunken eyes
- Dry lips/skin
- Dark concentrated urine or a strong smell
- Not passing much urine
- Feeling confused or irritable
- Feeling light headed
- Feeling light headed when standing up
- Thirst
What drinks can I have?
The drinks that you are taking may not be absorbed and will be passed straight out of the body. Salts such as sodium, potassium and magnesium, which have important roles, will also be lost through your stoma or fistula.
Ordinary drinks do not contain much salt. However, drinks that are more salty are better absorbed in your digestive system and help to reduce the output from your stoma or fistula. Drinking these may help prevent dehydration as fluid will move from your intestines into the rest of your body.
Ordinary drinks do not contain much salt. However, drinks that are more salty are better absorbed in your digestive system and help to reduce the output from your stoma or fistula. Drinking these may help prevent dehydration as fluid will move from your intestines into the rest of your body.
Examples of drinks that may need to be restricted:
- Coffee
- Tea/herbal teas/decaffeinated drinks
- Squash
- Water
An oral rehydration solution may be prescribed for you to help you re-absorb fluids from your intestines into your body. These drinks have a high salt content so are better absorbed.
Back to topDioralyte®
(Available on prescription) Mix 8-10 sachets in 1 litre (1000ml) of tap water or as advised by your dietitian.
St Mark’s electrolyte mix
Oral rehydration solution made at home and ingredients can be purchased from the chemist/ supermarkets/certain online retailers for less than the cost of a prescription.
20g (six level 5ml teaspoonful) of Glucose Powder
3.5g (one level 5ml teaspoonful) of Sodium Chloride (salt)
2.5g (half a heaped teaspoonful 2.5ml) of Sodium Bicarbonate (baking soda)
Mix all ingredients in 1 litre (1000ml) of tap water
Some patients may find it difficult to get used to the taste of oral rehydration solutions. Try the following tips to help:
- Add a small amount of No Added Sugar squash or cordial to the solution
- Drink the oral rehydration solution with a straw to help reduce the salty taste
- Keep the oral rehydration solution in the fridge to ensure it is cold
- Try alternative flavours
- A squeeze of fresh lemon/lime juice may be added
Try to avoid drinking around mealtimes as this can increase the output from your stoma or fistula.
When it is hot, we sweat and lose salt and water from our body. In this situation you may find it helpful to drink more of the rehydration fluids to replace the extra losses.
If you are given a fluid restriction and find it difficult to stick to this, try the following tips to help:
- Sip all fluids slowly through the day
- Use smaller cups/mugs/glasses for drinks
- Suck on boiled sweets or mints to keep your mouth from drying out
- Suck on ice cubes or ice lollies as part of your fluid allowance
If you are prescribed nutritional supplement drinks, or take drinks such as Complan or Build Up at home, please ask your dietitian which ones are most suitable for you.
If you wish to drink alcohol, check with your doctor if it is safe to do so as some medications can interact with this.
Some alcoholic drinks can increase your stoma output e.g. beer and lager, which may lead to dehydration. If you do drink alcohol, keep within recommended guidelines. You should not drink more than:
14 units/week with 2-3 alcohol free days. Spread the units evenly across the week. This guideline applies to both men and women
- 175 ml glass of wine (ABV 13%) = 2.3 units
- 1 bottle of wine (ABV 13.5%) = 10 units
- 1 pint of regular strength beer or lager (ABV 4%) = 2.3 units
- 25 ml single spirit (ABV 40%) = 1 unit
- 275 ml alcopop (ABV 5.5%) = 1.5 units
Which medications might help to reduce my stoma or fistula output?
There are some medications that can help to reduce your stoma or fistula output. These work by slowing down the passage of food and drink through the bowel (anti-diarrhoeal medication).
Examples include:
- Loperamide (Imodium)
- Codeine Phosphate
These medications may need to be taken around 30 – 60 minutes before eating to work best. You may also want to take a dose before a long journey or at bedtime if your stoma or fistula is very active overnight. Discuss this with your team.
Other medications work by reducing the amount of fluid your bowel produces (anti-secretory medication).
Examples include:
- Omeprazole
- Ranitidine
- Lansoprazole
- Octreotide, which may be switched to Lanreotide in the long term
If you notice medications in your stoma or fistula bag it is likely that these are not being absorbed. Speak to your doctor or pharmacist about changing the preparation.
The dose of medication may need to be increased over time to help reduce your stoma or fistula output. You may find that you are prescribed much higher doses than people without a high output stoma or fistula.
Back to topWhat should I do if I am losing weight?
If you find you are losing weight, you may need to increase your energy intake. To help with this, try the following:
- Try to have small, frequent meals and snacks, 5 – 6 times a day
- Snack on high energy foods e.g. full fat yoghurt, custard, mousse, cheese and biscuits, crisps or cake
Fortify your diet to gain extra calories from your food
Try the following:
- Add sugar, honey or syrup to cereals and puddings
- Add evaporated milk or cream to puddings, desserts and soups
- Grate cheese over potatoes and pasta
- Add margarine or butter to bread, teacakes and potatoes
Nutritious drinks such as milk or drinks made with milk e.g. drinking chocolate, milky coffee, milkshakes and malted drinks such as Ovaltine and Horlicks can be a valuable source of energy and protein. However, in some patients these can increase your stoma or fistula output. Please discuss with your dietitian.
If you have any further questions in relation to your diet and stoma/fistula output, please speak to your Dietitian who will be able to advise further
Back to top