What is the thyroid gland?
The thyroid gland is an endocrine gland. It makes hormones that are released into the bloodstream. These hormones travel in the blood and act as messengers to other parts of the body. They regulate the speed at which your body works. Therefore the thyroid gland keeps the body working at its normal rate.
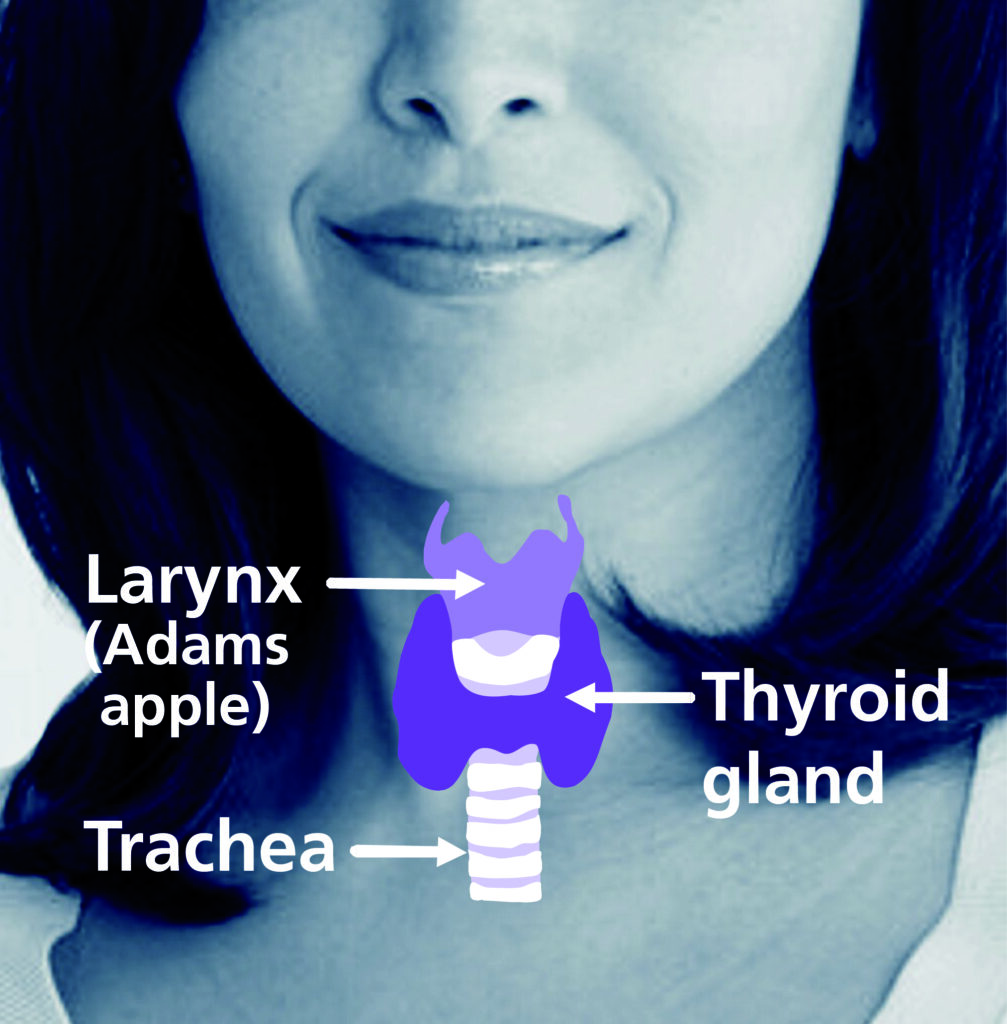
The thyroid gland is a small gland at the front of the neck, it has two lobes (each about the size of half a plum) which are joined together by a ridge of thyroid tissue called the isthmus. The two lobes lie either side of your windpipe (also called the trachea).
Below is an explanation of how the thyroid gland works
It is not essential that you know all this information but it may help you to understand why you have particular tests and treatments.
How is the thyroid gland controlled?
The hormones that the thyroid gland produces are called Thyroxine (T4) and Tri-iodothyronine (T3). The body needs a regular supply of iodine in order to produce these hormones. T4 contains 4 atoms of iodine and T3 has three atoms.
If the body detects low levels of these hormones in the blood, mechanisms are set in motion to produce more.
If there is too much of these hormones, less is produced until the levels return to normal. The body operates a fine balancing system and unless there are any problems you are mostly unaware of this process.
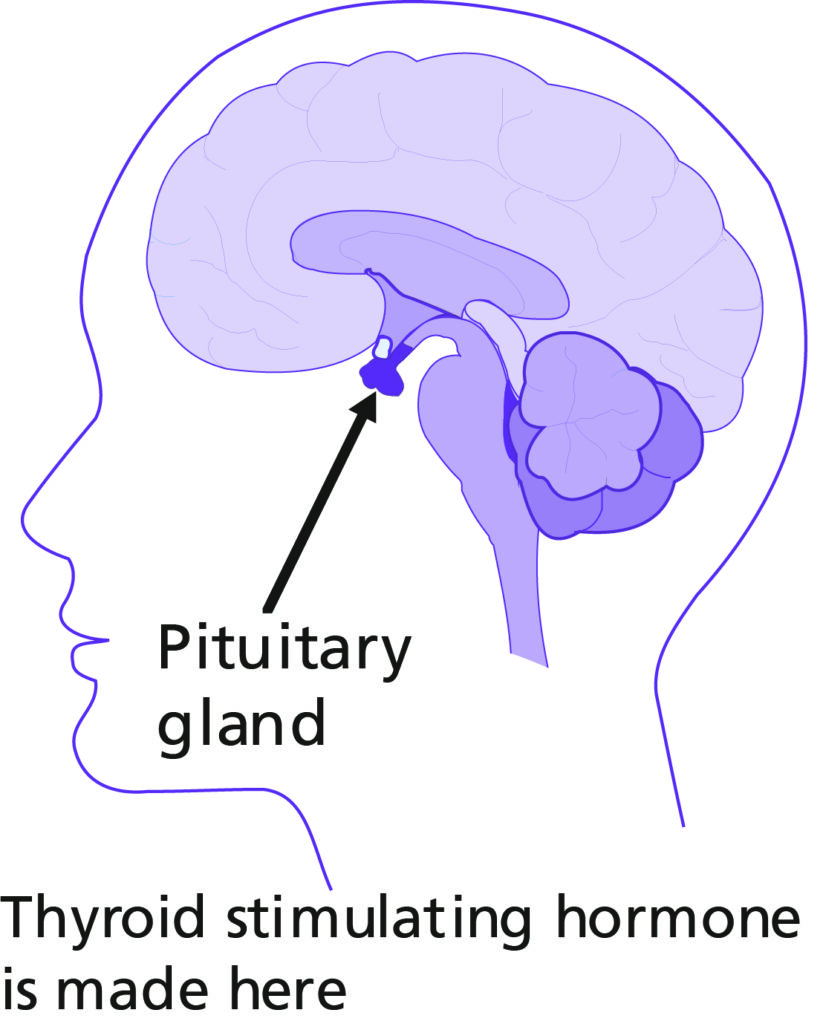
This balancing system works because the thyroid gland is linked to another gland called the pituitary; this lies underneath your brain in your skull. The pituitary senses the levels of thyroid hormones in your bloodstream. If the level of thyroid hormones (T3 and T4) are low, the pituitary secretes a hormone called ‘Thyroid Stimulating Hormone’ which is known as TSH. TSH stimulates the thyroid to take up iodine and secrete more T3 and T4. If the level of thyroid hormones rise above normal the pituitary stops production of TSH until T3 and T4 levels fall to normal. If the thyroid gland is unable to produce enough of these hormones (hypothyroidism) or the thyroid gland has been removed you will feel tired and lethargic and can put on weight easily.
If the thyroid gland produces too many hormones (hyperthyroidism) or you are taking too much thyroxine the opposite can happen and you can find it difficult to relax, have palpitations and an increased appetite. People loose weight or gain weight if they are taking too much thyroxine. Too much (as well as too little) T3 and T4 can also make you feel tired.
How is thyroid activity measured?
As well as an assessment of how you feel and a physical examination, a blood test can show how well your thyroid is working. These are sometimes called Thyroid Function Tests and measure the TSH level in your blood.
Cancer of the thyroid
Cancer of the thyroid is quite a rare form of cancer, although the number of cases are increasing which may be related to the increased number of scans performed or the improvements in the scanning equipment which can detect even the smallest abnormalities. It is usually slow growing and it may be some years before it starts to cause any noticeable problems.
What are the symptoms of thyroid cancer?
Sometimes there are no symptoms and the cancer is found by chance, however the following may occur:
- A painless lump in the neck which gradually increases in size.
- Difficulty in swallowing, due to the fact that the thyroid gland is close to the oesophagus (food pipe or gullet).
- Difficulty in breathing, because the thyroid gland is close to the trachea (windpipe).
- Hoarseness of the voice.
It is unusual for cancer of the thyroid to affect the production of thyroid hormones and give rise to symptoms of either hyperthyroidism or hypothyroidism.
How is thyroid cancer diagnosed?
Usually you attend your GP and he or she may refer you to hospital for some tests or for specialist advice.
Tests that may be included are:
- Fine needle aspiration or biopsy – for a fine needle aspiration a small needle is passed gently into the swelling in your neck. Cells are taken and examined under a microscope to check for the presence of cancer cells. The results usually take at least a week. Very occasionally a biopsy may need to be taken from the swelling when a small piece of tumour is sampled. This is usually done under an anaesthetic.
- Blood tests – blood tests are taken to check your thyroid hormone levels and your general health.
- Ultrasound thyroid scan – for this test gel is spread over your neck and a small device like a microphone, which produces sound waves, is then passed over the area. The sound waves bounce off the tissues in the body to produce echoes which are converted into a picture showing the inside of your neck.
- CT scan – this uses a collection of x-rays to build up a more in-depth picture of a part of your body. You will not feel anything while having the procedure.
- MRI scan – this uses a magnetic field and radio waves to produce detailed pictures of a part of your body. You do not feel anything while you are having the scan, but you will hear a loud rhythmical banging noise.
Are there different types of thyroid cancer?
There are four types of cancer of the thyroid called papillary, follicular, medullary and anaplastic cancer. By removing some cells from the gland and examining them under a microscope the doctor will be able to tell you which type you have and, therefore, decide on which kind of treatment will help you the most.
- Papillary is the most common type, it is more common in younger people particularly women.
- Follicular is less common and is usually found in slightly older people.
- Medullary is a rare type, which sometimes runs in families.
- Anaplastic is usually found in older people and is more common in women. It tends to grow more quickly than the other types.
Papillary and follicular cancers are sometimes called ‘differentiated thyroid cancer’ because they look and act like normal thyroid cells and concentrate iodine. This means they can be treated with radioactive iodine also known as radioiodine therapy. If you want information about radioiodine please ask for a leaflet. Radioiodine is usually given after surgery if required.
What causes thyroid cancer?
The cause of thyroid cancer is not known, but research is on-going to try and find this out. Occasionally it is found in people who have had radiotherapy to the neck 10 to 20 years ago. Very occasionally it is hereditary. Please ask about this if you are concerned.
Thyroid cancer treatment and targeted drug treatments
What types of treatment are used?
Surgery, radioactive iodine therapy, external beam radiotherapy, hormone therapy and the radioactive iodine treatment can be given a number of times if needed and are given alone or in combination to treat thyroid cancer. After treatment, patients with thyroid cancer are usually cured. If the cancer has spread to other parts of the body (which is rare) there is still a good chance of cure. Some thyroid cancers can return, especially in the very young, the elderly and in those with advanced disease at presentation. Even if thyroid cancer returns, it can usually be effectively treated the second time around. It can return at any time so lifelong follow up is important.
All patients who have been diagnosed with thyroid cancer will be discussed at a multi- disciplinary team meeting (MDT). This consists of a group of professionals including your consultant, who meet on a regular basis to discuss the best plan of treatment for their patients. The evidence for and against further treatment is discussed and the potential benefits and disadvantages.
Your doctor will then plan your treatment by taking a number of factors into consideration, including your general health, the type and size of the tumour, and whether it has spread beyond the thyroid.
The most common treatment route includes surgery, this may be followed by radioactive iodine treatment (internal radiotherapy).
Surgery
The first treatment for thyroid cancer is usually an operation. Some people only have part of the thyroid removed. If only one lobe of two is taken out, the operation is called a lobectomy. If all the thyroid gland is removed it is called a thyroidectomy. The thyroid gland is looked at very carefully under a microscope after the operation.
The choice of further treatment will depend on the type and size of the cancer found.
Side-effects of the surgery may include:
- Your voice may sound weaker for some time afterwards.
- Your neck may feel stiff and sore.
- There may be some damage to the parathyroid glands, the tiny glands behind the thyroid. Their function is to control the level of calcium in the blood. Therefore you may require calcium supplements, but this is usually only for a short time. If your calcium level is low you can feel unwell and develop tingling in your hands, feet or face.
- If all the thyroid gland has been removed you will require thyroid hormones following surgery. Some patients also require radioactive iodine treatment, external beam radiotherapy or both.
Clear recommendations for and against further treatment after surgery is decided for certain groups of patients. However there is a group of patients where overall benefit of further treatment is uncertain. In these circumstances personalised decision making is recommended.
What is personalised decision making?
This is where you are given all the information about the implications of different treatment options will have the opportunity to discuss this with your consultant. Your specialist nurse will also be available to help you with information and choices. It is important to remember there is no right or wrong decision in these cases. The decision will be a shared one between you and your doctor.
What should I consider?
It is important to make sure you understand why the evidence for or against further treatment is inconclusive. Personal feelings in these cases are very important; don’t be afraid to say how you feel. Also think about how further treatment will affect your social/work circumstances.
If you and your consultant come to the decision that it is in your best interests not to have further treatment you will still be followed up with blood tests and in some cases scans to ensure all remains well. If you decide in the future you would like to discuss further treatment again please do not hesitate to contact your consultant or nurse specialist.
Radioactive iodine therapy
(also called radioiodine treatment)
This form of treatment consists of swallowing a radioactive iodine capsule and the iodine is taken up by the thyroid gland. Radioiodine is used with papillary and follicular thyroid cancer. The small dose of radiation is concentrated in the thyroid cells and destroys them. It is a way of giving radiotherapy internally.
If you are to have Radioactive Iodine Therapy you will be given a leaflet with more information.
What does it mean if someone says I am radioactive?
Everyone comes into contact with a very small amount of radioactivity during his or her life. You can’t see it, but scientists can measure it with special instruments. Some people receive more radiation than others simply because of where they live and what they do. These amounts are still very small. Radiation can be very useful. It can be used for patients with thyroid cancer to kill the cancer cells as part of their treatment.
When radioactive iodine is given to a patient it is absorbed into their body and they are called ‘radioactive’. There are very strict laws surrounding the use of radioactive substances. Although the amount of radiation present in someone after they have swallowed the capsule is small, it makes sense to limit their contact with other people because of the radioactivity.
That is why when you have the treatment you are kept in your own room and the amount of time people can spend with you is carefully monitored. Pregnant women and children are more sensitive to the effects of radiation, therefore there are stricter rules for these people and they are asked not to visit at all while you have treatment. You may also have restricted contact for a time after discharge.
External beam radiotherapy
This type of radiotherapy is used less often than radioiodine for thyroid cancer. It can be used to destroy any cancer cells that do not take up and respond to radioiodine. If you are to have radiotherapy you will be given a leaflet with more information.
Targeted drug treatments
Sometimes, despite having radioactive iodine, the cancer spreads to other areas such as the lungs and other treatments may be considered. This is the case if the cancer stops responding to the radioactive iodine given before. You can be treated with a targeted drug called a TKI (Tyrosine Kinase Inhibitor) These are tablets taken every day at home that can help to control the cancer. Like all tablets, there are side effects and you will be seen frequently by your doctor and nurse to monitor these.
Thyroid hormones
If you have had all your thyroid gland removed your treatment will include taking thyroid hormone tablets (levothyroxine) for the rest of your life. This is because once you have your thyroid gland removed you can no longer produce the hormones your body needs. Without these hormones you would develop signs of hypothyroidism.
You will have regular blood tests to make sure you are taking the correct amount and that the thyroid stimulating hormone (TSH) is suppressed (at a low level). It can take a while for your body to adjust to the hormones and, the strength (dose) of your tablets may change a few times in the first year or so (usually in 25 microgram steps). It takes around six weeks for the TSH to stabilise after starting thyroxine or after changing the dose; therefore blood tests are usually done six to eight weeks later. Eventually you should only need a blood test once a year (more often for pregnant women).
Please let us know if you are having palpitations because this may indicate that the dose of thyroxine is too high for you.
Why is it important to take the right amount of thyroid hormones ?
This paragraph only applies to papillary and follicular thyroid cancer. It is essential that you are taking enough thyroxine because if you take too little, your body will produce more TSH which can stimulate the papillary and follicular thyroid cancer cells to grow. The amount of TSH can be measured by a blood test. For a time the level of TSH needs to be lower in patients who are to have radio iodine treatment. You will have an ultrasound scan or a radio iodine scan 9-12 months after treatment. If the result is satisfactory and your thyroglobulin results are undetectable your consultant will then adjust the target level for your TSH and you will be discharged to the care of your endocrinology team. Your family doctor (GP) will be informed of the TSH levels required but may need to be reminded of this if they adjust the dose of your thyroxine. Because thyroid cancer is very rare, GPs only occasionally see patients in your situation.
Follow-up clinics to monitor treatment
Most patients attend follow-up clinics with their oncologist in Leeds and also their surgeon or endocrinologist (hormone specialist). If you are not already seeing an endocrinologist we will usually refer you to one at your first visit to the Leeds Cancer Centre after radioiodine treatment. Appointments are usually alternated between your oncologist and endocrinologist. The time between clinic appointments increases as time goes on. Sometimes the follow up appointments will be arranged as a telephone call, but blood tests may be arranged before the appointment to check the thyroid function and thyroglobulin and the results will be discussed at your appointment.
Thyroglobulin
What is thyroglobulin?
Thyroglobulin is a protein that can be measured by a blood test. It is made by normal thyroid cells and thyroid cancer cells. Papillary and follicular thyroid cancer cells produce thyroglobulin but medullary and anaplastic thyroid cancer cells do not. After surgery and radioiodine treatment, the thyroglobulin level is usually very low. If the amount of thyroglobulin in the blood is high, there are usually some thyroid cancer cells present (requiring more treatment). It is useful to measure the thyroglobulin in your blood at least once a year. Thyroglobulin level results take up to a month to return from the laboratory. Some people have antibodies to thyroglobulin and thyroglobulin cannot be measured in this situation. For these patients we sometimes need to do extra scans and continue to see you in the oncology clinic.
Useful addresses for support and information
The Nuclear Medicine Therapy Team
Leeds Cancer Centre,
Nuclear Medicine Department
Level 1, Bexley Wing, Leeds LS9 7TF
Thyroid Oncology Nurse Specialist Team
Leeds Cancer Centre,
Level 6, Bexley Wing, Leeds LS9 7TF
Leeds Cancer Support
Leeds Cancer Support complements care provided by your clinical team. We offer access to information and a wide range of support, in a welcoming environment for you, your family and friends. We can be found in the information lounges in Bexley Wing and also in the purpose built Sir Robert Ogden Macmillan Centre.
The Sir Robert Ogden Macmillan Centre
The Centre is on the St James’s Hospital site and offers a variety of support services including complementary and supportive therapies. These therapies include Reiki, relaxation and visualisation, hand and foot massage and many others. We also offer a weekly exercise class and a monthly support group. You can just drop in for a coffee and a chat anytime.
Contact numbers for Leeds Cancer Support
Information Lounge Level -2 Radiotherapy Department
Open from 8.00am – 6.00pm Tel: (0113) 206 7603
Information Centre Level 1 Outpatients Department
Open from 10.00am – 4.00pm. Tel: (0113) 206 8816
Sir Robert Ogden Macmillan Centre
Open from 10.00am – 4.00pm. Tel: (0113) 206 6498
All the above services can be emailed on:
Maggie’s Centre
A warm, welcoming place where you can meet people who are experiencing similar things to you. You may also be able to find support groups specific to your needs and get advice and information from their professional staff.
You don’t need an appointment and all support is free.
Open Monday to Friday 9.00 am – 5.00pm. Tel: (0113) 427 8364
Address: St James’s Hospital (next to the multi storey car park), Alma Street, Leeds LS9 7BE
Email: [email protected]
Website: maggiescentres.org
Thyroid cancer groups
Butterfly Thyroid Cancer Trust
This is a voluntary support group for patients affected by thyroid cancer based in Newcastle. It is a patient-led group and they are happy to receive calls and emails from Leeds patients.
Tel: 01207 545469 Website: www.butterfly.org.uk
Email: [email protected]
The British Thyroid Foundation
This group deals mainly with patients that are hypo- and hyperthyroid. We advise asking to speak to the thyroid cancer expert for information and support. Suite 12, One Sceptre House
Hornbeam Square North, Hornbeam Park, Harrogate, HG2 8PM
Tel: 01423 810093 Website: www.btf-thyroid.org
Support group for patients with medullary thyroid cancer called AMEND (Association for Multiple Endocrine Neoplasia Disorders)
Email: [email protected] Tel: 01892 516076/841032
General cancer information organisations
Macmillan Cancer Support
Open 9am to 6pm Monday to Friday. A textphone service for deaf and hard of hearing people is also available.
Freephone: 0808 808 0000 Textphone: 108001 0808 808 0121
website: www.macmillan.org.uk
If more information is required:
- Guidelines for the management of thyroid cancer (2014) and patient information booklets (similar to the Leeds information leaflet) may be downloaded from the British Thyroid Association www.british-thyroid-association.org
- Medline (search the medical literature) www.medlineplus.gov/
- Cancernet www.thyroid-cancer.net/