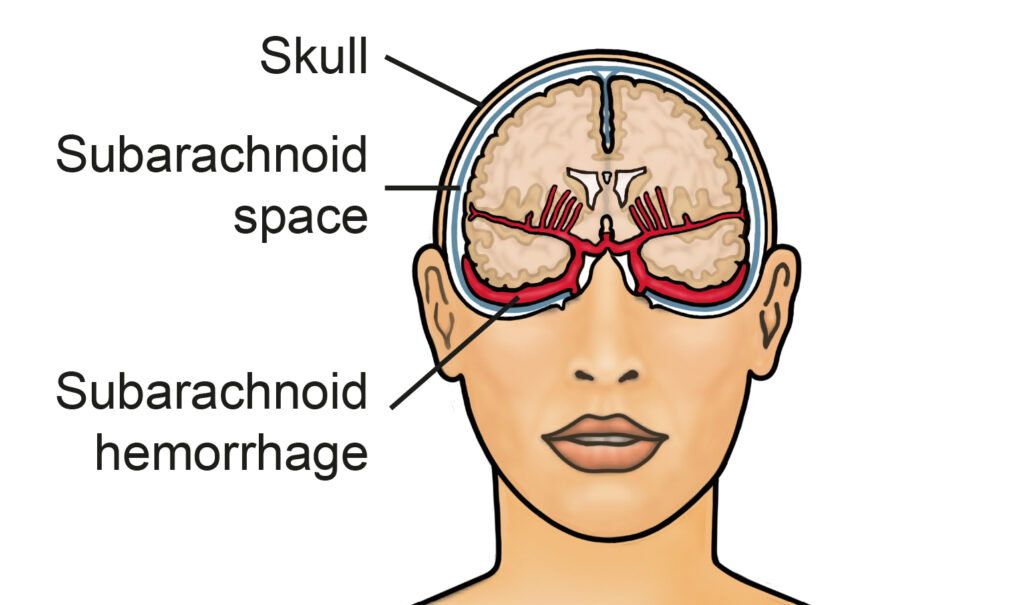
What is a subarachnoid haemorrhage?
A subarachnoid haemorrhage (SAH) is a bleed in between the layers that cover the brain, the area where the blood leaks into is called the subarachnoid space.
The bleeds can happen as a result of trauma, or they can be spontaneous (happen without warning). Spontaneous SAH is most commonly due to a ruptured brain aneurysm but other vascular malformations can also cause the conditions. In some cases of spontaneous SAH, no cause/anomaly is found.
Symptoms of a SAH are a sudden onset of ‘thunderclap’ headache, nausea (feeling sick) and vomiting, neck stiffness, confusion, photophobia (sensitivity to light) and visual changes. More severe symptoms include seizures (fits) and loss of consciousness.
Are there any warning signs?
There are usually no warning signs of the aneurysm until it bursts/ruptures. In some rare cases a large aneurysm can press on areas of the brain causing symptoms.
Diagnosis
You will undergo a CT head scan to diagnose a subarachnoid haemorrhage. In some cases if your CT scan looks OK but we still suspect a SAH clinically, you may undergo a lumbar puncture. This involves taking some fluid out of the spinal canal to see whether there is blood products circulating within the cerebrospinal fluid which can help make the diagnosis of SAH.
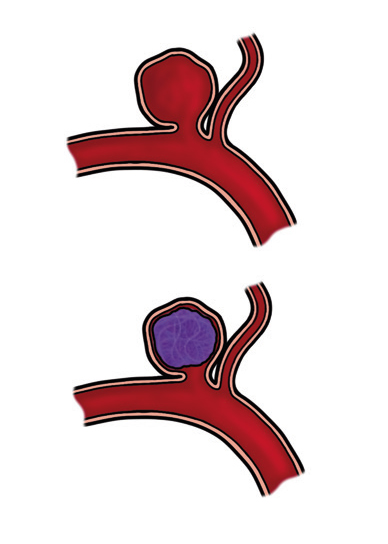
Once we have diagnosed you with a SAH we will need to perform tests looking at the blood vessels supplying your brain to find the cause of the bleed, these are usually a CT angiogram (CTA) and/or catheter angiogram. Most importantly, we are looking for an abnormality called an aneurysm. This is a weakening on an artery wall that often looks like a blood blister.
If we discover that the cause of the bleed is due to a burst (ruptured) aneurysm there are a number of different treatments we can perform to fix it and stop the aneurysm from re-bleeding.
What is an aneurysm?
An aneurysm is a bulge in a blood vessel caused by a weakness in the vessel wall. Over time the pressure of the blood passing through the weakened vessel causes a small area of the wall to bulge outwards. A SAH occurs when the weakened vessel wall ruptures due to the pressure of the blood. This results in blood escaping from the vessel into the subarachnoid space.
It is not fully known why people develop aneurysms and in most cases there is no way of identifying the people who are at risk of developing them. Research has suggested that SAH are more common in women and in people aged 40-60.
Other factors that increase the risk of aneurysms forming are high blood pressure, smoking and excessive alcohol consumption. There are a small number of people who have a inherited genetic risk of developing cerebral aneurysms but this risk is small. If you have two or more immediate family members (sibling, parent or child) speak to your nurse specialist about MRI screening. Certain connective tissue disorders can increase risk such as polycystic kidney disease, Ehlers-Danlos syndrome and Marfans syndrome.
It is important to note that most people develop aneurysms with none of the above risk factors.
Treating the aneurysm
There are a number of ways your aneurysm can be treated. There are endovascular and surgical options. Treatment depends on the size, shape and position of the aneurysm which can influence the risk of it bleeding over your lifetime. Most ruptured aneurysms are treated endovascularly.
- Coiling, stenting and the use of WEB and Contour devices are endovascular procedures which are performed in Radiology theatres by an Interventional Neuroradiologist. These are performed by accessing the aneurysm from inside the blood vessel via the groin.
If a cerebral stent is required to treat your aneurysm, you will be commenced on a course of dual anti-platelet medication (blood thinners) for a period of time. Usually after several months one of these medications can be discontinued, and the other medication (usually Aspirin) will continue lifelong. Your
Consultant and nurse specialists will counsel you about dual anti-platelet medication should you require this.
This mode of treatment avoids the need to open up the skull. You will need to return to hospital for follow up scans to ensure the aneurysm remains fully treated. These scans are usually performed at 6 months and 2 years post procedure.
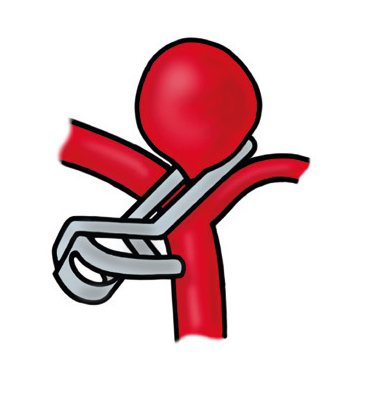
- Surgical Clipping – this is performed by a Neurosurgeon who will make an opening in the skull (craniotomy) to access the aneurysm and place a metal clip around the neck of the aneurysm to prevent blood from entering it. This is a permanent treatment of the aneurysm. You do not usually require follow up scans following an aneurysm clipping, unless you have multiple aneurysms.
There are risks involved with any procedure but it is very likely that the benefits of your treatment outweigh the risks. Your doctor will discuss these with you fully before you give consent to proceed with the treatment. In the event you cannot consent to treatment due to emergency/low conscious levels treatment will carried in with your best interests.
Complications in Hospital
Hydrocephalus
After a SAH, there is a possibility that the fluid around the brain can build up, this is because the fluid pathways can become blocked with the blood over the surface of the brain. When the fluid builds up it can make a person very unwell. This can be treated with the insertion of a drain to take away the excess fluid. The drain can be placed in a person’s head (EVD) or lower back (lumbar drain).
This is usually a temporary measure until the person is no longer reliant on the drain. In a small number of cases people will need a permanent, internal drain inserted
(a ventriculo-peritoneal shunt). If this is required your surgeon will explain how the drain will work, and you will receive advice and support from the hydrocephalus specialist nurse.
Delayed cerebral ischemia (DCI)
DCI can occur when there is a reduction in blood supply around the brain. This can cause stroke like symptoms which can occur gradually and are usually temporary but can become permanent if an area of the brain does not get enough oxygen. A possible cause of DCI is vasospasm where the vessels in the head can become narrower, reducing the blood flow around the brain.
Vasospasm is usually medically managed but if severe, treatment can be given in radiology theatres. You will be started on a 21 day course of medication called Nimodipine to help prevent vasospasm from occurring. Your nurse specialists will also carry out ultrasound imaging on you head called trans cranial dopplers to assess the vessels for spasm.
Hyponatremia (Low Sodium)
Hyponatremia following SAH can occur due an increased loss of sodium in the urine called cerebral salt wasting (CSW) syndrome or sometimes due to an inappropriate antidiuretic hormone secretion (SIADH). You will have regular bloods taken to check your sodium levels whilst in hospital, and if you do develop low sodium we can give you medication to correct this. The condition is temporary but may lengthen your hospital stay until your sodium levels are corrected.
Recovery
After a subarachnoid haemorrhage you may experience one or more of the following symptoms, everybody is different and recovers at their own pace:#
Headaches
Headaches are a common feature in recovering from a SAH. In the first few days they are usually severe and fairly constant. This is due to the blood around the brain causing on-going irritation. Eventually the blood products will be broken down and reabsorbed by the body; this can take a few weeks.
The frequency and severity of headaches usually improve over time; the time varies from person to person. People often find in the first few weeks of going home that headaches are triggered by tiredness or periods of concentration.
You will be discharged home with pain relief which should be taken as prescribed. People are understandably anxious about experiencing on-going headaches, and associate them with concern over having another SAH. Headaches are very common in the recovery from a SAH but if you are concerned contact your GP or nurse specialist.
(Fatigue) Tiredness
Fatigue can be described as overwhelming physical and mental tiredness and is a very common feature in recovering from a SAH. For some it may feel like overwhelming tiredness, which makes them unable to complete normal activities of daily living. People may say they feel exhausted, lacking in energy, weak, unable to motivate themselves, or sleepy. For others it may worsen difficulties associated with their SAH, for example, forgetfulness or dizziness.
You may require a daily rest period in the first few weeks of recovery and it is important to listen to your body. Fatigue improves over time and you will gradually be able to return to your previous activities but this can take some months.
Back pain
People can experience lower back pain following a SAH for a number of reasons. This could be due to lying in bed for long periods of time with little physical activity. This will begin to improve as you increase your activity.
The blood from your SAH can circulate in your spinal fluid causing irritation of the nerves leading to lower back pain and shooting pains down your legs. Although this is unpleasant it will resolve over time and can be managed with pain relief.
Cognitive (thinking difficulties)
Cognition describes brain functions such as memory, concentration, information processing, decision making and general thought processes. Any one of these functions can be altered after a SAH and you will receive support from the occupational therapists during your hospital stay who will carry out an assessment and advise you with strategies on how to manage any difficulties in relation to your daily activities.
Short term memory can be affected after a SAH, especially in the early days after the bleed. Many people can’t remember their first few days in hospital and some people remember little about their hospital stay. Memory usually improves gradually but in some cases there can be permanent changes seen. People tend to find that their memory may become worse when they are tired. Strategies to help manage your short term memory can be making lists, leaving prompts around the house, using diaries and calendars and keeping distraction to a minimum to help you maintain concentration.
Emotional difficulties
Having a SAH is a sudden, unexpected major life event and people can find it difficult to come to terms with. People describe feeling emotional, depressed, tearful, anxious and angry sometimes for no apparent reason. These feelings can be physical (related to the injury to your brain from the bleed) or emotional (a reaction to a traumatic experience). In some cases people can experience depression and anxiety or both.
If you are struggling with your mood it is important to speak about how you feel with your friends and family. If you are concerned or feel you might benefit from some trained support, speak with your GP or your nurse specialist.
Going Home
Going home can feel daunting after a SAH and it takes time to adjust. There is no set time scale on recovery and you will likely have good days and bad days. Remember to listen to your body and don’t be hard on yourself, recovery takes time.
Work
We advise you to take 6-12 weeks off work, depending on how you feel and what you do for work. Ask your doctor for a sick note before you leave hospital. It is advised that when you do return to work, that you make a phased return.
Driving
Depending on what treatment you have had, you may be required to notify the DVLA of your hospital admission. Either way you must not recommence driving until you are deemed clinically recovered by a healthcare professional. Speak with your nurse specialist about driving specific advice.
Smoking
As smoking is a known risk factor in aneurysms forming and rupturing we strongly advise that you consider stopping smoking. You can access smoking cessation services through your GP.
Going on holiday
You are safe to fly once you feel well enough to do so, if you are unsure about this speak with your nurse specialist. There are no restrictions on flying and your aneurysm coils/clips will not be affected by the airport security machines and will not set them off. It is advisable to notify your travel insurance provider of your recent hospital stay.
Meet the Team
Consultant Neurosurgeons:
- Mr Kenan Deniz
- Mr Ian Anderson
- Mr Asim Sheikh
- Mr Atul Tyagi
Consultant Interventional Neuroradiologists:
- Dr Tufail Patankar
- Dr Nayyar Saleem
- Dr Tony Goddard
Neurovascular Nurse Specialists:
- Mrs Hannah Dawson
- Mrs Sharon Sullivan
Neurovascular MDT Coordinator:
- Miss Vanessa Moss