All about me is an interactive tool, for those attending the infection clinic, to enable further discussion with professionals involved in your care.
You should be given a printed copy of this by your nursing team. Please speak to them if you have not received it.
What do you know so far?
Welcome to your new clinic pack! Inside you will find lots of information about why you come to clinic and who you will meet along the way. This is your very own pack and we will add to it together during your time with us. We can decide together whether your pack will be kept safe in the hospital or if you would like to take it home.
Back to topHere are some reasons we like to see you in clinic…
- To see how you are growing and to check that you are well.
- To talk about your health information that is private to you.
- To ask how you are feeling.
- To talk about any medicine you may be taking.
- To have a blood test.
- To help you in other things that you do, for example, school, friendships and activities.
What’s inside my blood?
When you come to clinic, you may be asked to have a blood test. This is so we can look
closer inside your blood to help us know what is happening in your body.
We use something called a microscope, which is a magnifying glass that
makes tiny things look bigger.
These are some of the cells we see in your blood, let’s talk about the
very important jobs that they do:
- Platelets – these cells help our blood stick together after we have hurt ourselves.
- Red blood cells – these cells give us energy and carry oxygen around our body. This helps us to run and jump and play.
- White blood cells – these are our body’s cells, that stop us getting unwell or help make us feel better.
Did you know?
There are around 250 million red blood cells in just one drop of blood!
What else might be seen in my blood?
There may be other things in your blood. For example, a virus.
There are different types of viruses:
- Some stay in our body for a short time and make us feel unwell, like a cough and a cold.
- Others live in our body but don’t grow or make us feel poorly.
You can’t always tell when someone has a virus in their blood. This is because the virus can be very small and quiet and may not cause any problems, especially if you look after yourself and come along to clinic, just like you do!
Did you know?
Have you ever had chicken pox? This is a virus that will always stay in your body even when your spots and itchy rash have gone away.
Did you know?
Some microscopes can magnify a virus up to 400 times its original size. Imagine looking at an ant the size of a building!
What is an immune system?
An immune system is the body’s protection against different types of bacteria and viruses, that can make us unwell. Your white blood cells are part of the immune system. One type of white blood cell you will hear us talk about is the CD4 cells.
Did you know?
Laughter can boost your immune system!
Living with a virus
We know that viruses that live in our body are very small and that we wouldn’t even know they were there. Sometimes viruses stay in our body and because you have a certain virus that stays in your body, you come to see us in clinic. This means we can work together to help you stay well and make sure the virus stays small. Your immune system will need a helping hand to protect you, and this is why you will need to take medicine every day.
Remember, people will never know that you are living with a virus, and it shouldn’t stop you going to school/ college, having fun or anything else you want to do!
Back to topTalking about your health
There may be times when you have some questions or want to talk about your health, your appointments or your medicines. It’s important to think about who the best people are to ask these questions of, as not everyone understands about health and medicines.
In the box below please draw round your hand. Now let’s write the names or draw pictures of five people who you can talk to about your health and medicine. This will help make sure you get the right information and the right support.
You now know the name of your virus
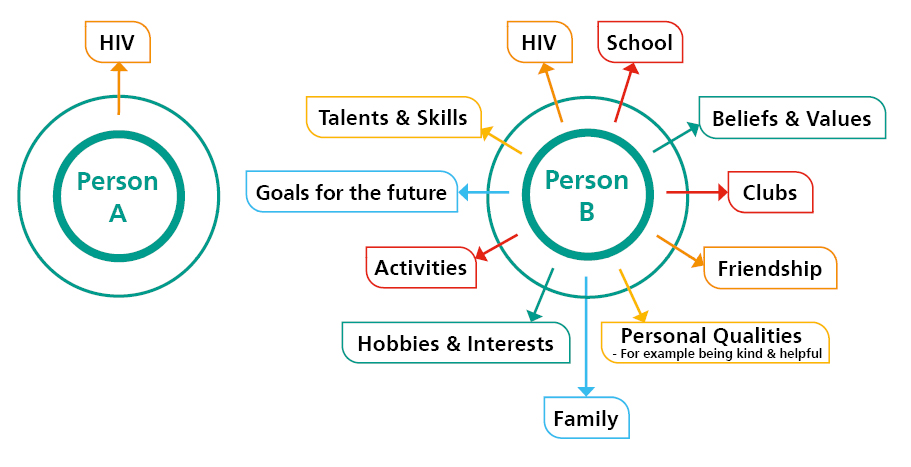
You now know that your virus is called HIV. As we have talked about together this stands for Human Immunodeficiency Virus and we will go into detail on the next pages. For now, it is important that you know, having HIV does not define you and you can live a long, happy and healthy life alongside HIV.
Have a look at the two diagrams. Person A and B both live with HIV. However, for Person B the HIV appears to be a smaller part of their life because of their focus on the many other things in their life.
Did you know?
There are currently around 326 children and young people being treated for HIV in the UK (CHARS and UKHSA data 2024).
Over the last 20 years more than 2,000 children and young people have been diagnosed and many of them are now adults.
Did you know?
There were 94,397 people living with diagnosed HIV and accessing care in England in 2022 www.gov.uk Ask your clinic team about your local area
Did you know?
People living with HIV can have a normal life expectancy!
What is HIV?
HIV (Human Immunodeficiency Virus) is a virus that attacks the type of white blood cell called a CD4 cell. These are part of your immune system and help you stay healthy by fighting off infection and illnesses.
The HIV virus destroys these cells, using them to make copies of itself. These copies then get into other CD4 cells and destroy these, until your immune system becomes too weak to protect you from infection. This can develop into advanced HIV, also known as AIDS (Acquired Immune Deficiency Syndrome).
Two important Blood tests:
Viral load?
This test shows the level of HIV in your blood. Results are given as copies per millilitre (copies/mL) and it will tell you how well your HIV medicines are working. The aim is to reduce this to less than 50 copies/mL.
CD4 count?
This tells you how healthy your immune system is. Results are shown in cells per cubic millimetre (cells/mm3) – the higher the CD4 count, the better.
Did you know?
World AIDS Day is celebrated on the 1st December each year!
My results chart – Viral load
You can plot your results on the chart provided within the printed booklet.
Back to topMy results chart – CD4
You can plot your results on the chart provided within the printed booklet.
Back to topHow do my medicines work?
If you are living with HIV, you can take medicines every day to prevent HIV damaging your immune system and keep you healthy. You will know your medicine is working when your viral load, the level of virus in your blood, gets very low. This is called being ‘undetectable’. Currently, there is no cure for HIV, but taking medicine regularly means you can expect to live a healthy life.
Your doctor will usually recommend a combination of three types of medicine (triple therapy), which work together to reduce the amount of HIV in your body. You will usually be able to take all your medicines in one combination tablet. There are also now HIV medicines that can be taken as an injection, but these aren’t yet available for everyone.
For more information on the different types of medicines and how they work please read the ‘My Meds My Health Booklet’ on the Chiva website:
www.chiva.org.uk/hiv-information/medication-2/
Did you know?
There are free downloadable apps to help remind you when it’s time to take
your medicines. Please ask your clinic team for details.
My Treatment
When do I start treatment?
It’s recommended you start taking medicine as soon as you are diagnosed with HIV. The sooner you start, the better, as it will protect your immune system and stop you from getting unwell. But this may be delayed if there are other conditions to treat first.
How long will my medicines work?
You could be on the same HIV medicine for many years, even your whole life.
Can I change medicines?
Yes, you can change medicines if you want to, particularly if you have unwanted side effects, or your combination doesn’t suit your lifestyle. Finding what works for you is important – talk to your doctor, nurse or pharmacist. They can monitor any side effects and help make sure you are on the right combination for you.
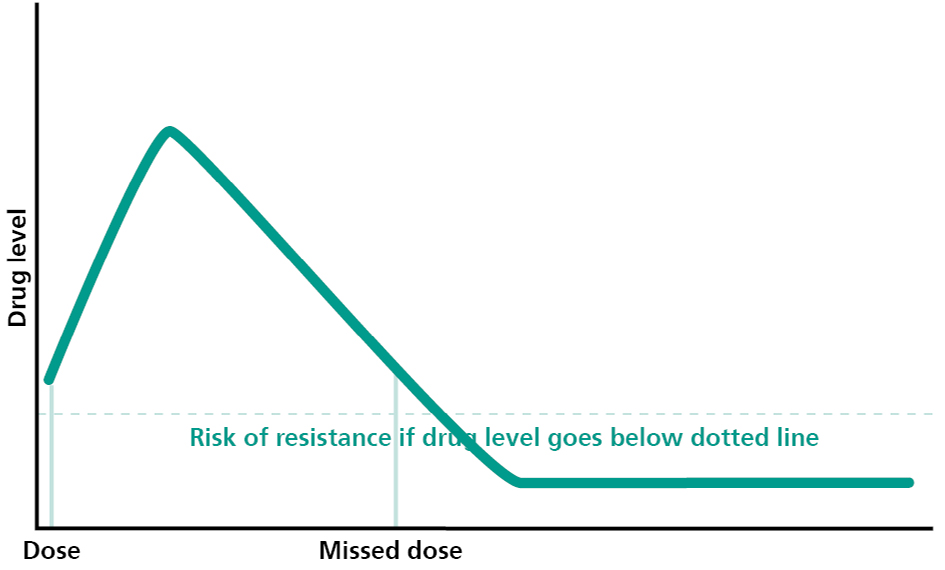
Can I stop taking my medicines?
Once you’ve started taking medicine, try not to stop, unless there’s a serious reason. Your viral load will increase again after only a few days without medicine. And there’s a risk your body will build up resistance to certain drugs, which can leave you with fewer options for treatment.
Stopping medicine should always be discussed with your clinic, and if you do stop, it’s important your CD4 levels and viral load are carefully monitored.
What if I forget?
If you forget to take your medicine, don’t worry. Most people will be late with their medicine sometimes. Just take it as soon as you remember. However, don’t take it if you only realise a few hours before you’re due to take the next tablet. It’s not good to take a double dose as you might experience more side effects. Whilst the very occasional missed dose is unlikely to cause you any problems, regularly forgetting or choosing not to take your medicine can cause serious problems. If you are missing doses regularly, it’s important you speak to your clinic team to explore reasons, get support, and find solutions.
Did you know?
If you are struggling to swallow or take your medicine, please talk to your clinic team as they have lots of top tips!
Young people’s top tips to help you remember your HIV medicines!
The young people of the Together 4 Life group in Leeds came up with these tips to help when taking HIV medicines:
“Attending a support group has helped me see that there are others who find taking medicines difficult”
“Take your medicines alongside other daily routines. e.g. brushing your teeth”
“Ask a family member or someone close to you to remind you”
What do the young people of Chiva say about taking medicines?
Chiva is a registered charity working across the UK and Ireland improving care for children and young people living with HIV and their families. Chiva provides information, guidance and support for professionals, parents and young people living with HIV and runs an annual support camp for children and young people living with HIV.
Chiva have a fantastic website with lots of free resources, top tips and hints especially for young people who want to know more about living with HIV. Go to www.chiva.org.uk and have a look!
Here are some top tips from the young people of Chiva and what they said about the positive aspects of taking medicine:
“Keeps your immune system healthy and your HIV virus low”
“Keep an emergency supply where you might need them”
“Makes it more difficult to pass HIV on to others when you take your HIV medicine”
“Take your medicines with something that tastes good to disguise the taste”
“Helps you live a normal life”
“Use an alarm on your watch or mobile phone as a reminder”
“Ask your clinic staff for a weekly pill box/ dosette box”
“If you think you have any side effects, your clinic team will help you”
“Medicine prolongs your life”
“Reward yourself with a treat when you have done well”
“Be involved in making decisions about your treatment”
“Have an answer ready just in case someone asks why you are taking medicines”
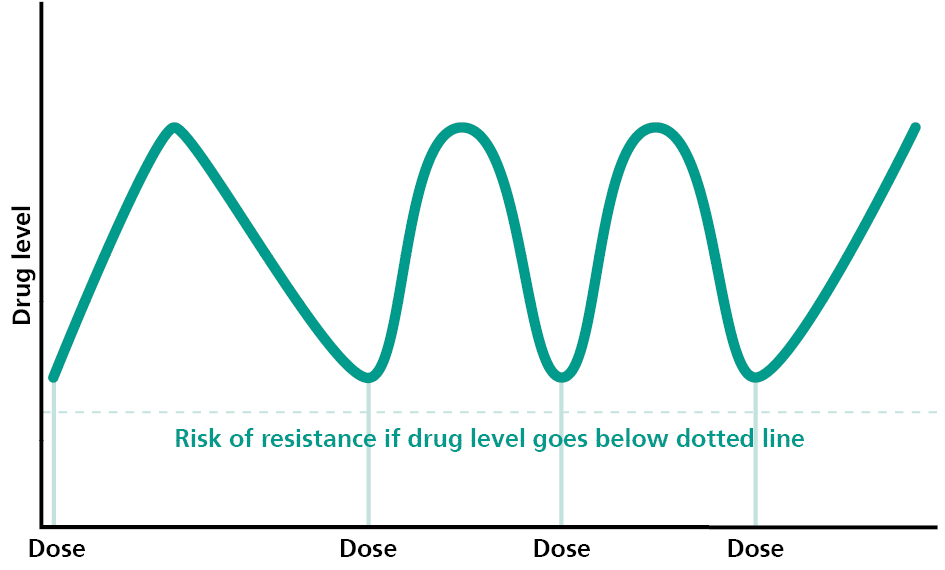
What is drug resistance?
Resistance is when something slows down and stops working as well as it should. Sometimes this happens with medicines and is known as drug resistance. It occurs when the virus changes its structure in a way that stops the medicine from working. These changes are called ‘mutations’.
There is a risk of resistance when your medicine levels drop. This can be as a result of incorrect doses (e.g. while you are growing) or missed doses (e.g. forgetting) or because of a drug interaction that can affect concentrations of your HIV medications, that is why it is always important to tell someone in your medical team if you start a new medication, even if it is something you buy in a shop or a vitamin preparation. If your viral load increases on treatment this could be as a result of drug resistance.
Did you know?
Once resistance has occurred it will always be there and will limit your future treatment options.
How can I avoid resistance?
As we have talked about previously, taking medicines as advised by your clinic team is important. This is also the best way to avoid resistance. This will allow your medicines to work for many years.
Resistance can be difficult to understand at first. Read the story below and think about the various obstacles that prevent the car from working as it should.
Imagine you are on a long car journey. It a nice calm day and the road ahead is clear. As you travel along you notice the road gradually starts to get bumpy and obstacles begin to appear. You are running low on petrol but decide to continue your journey without filling up. Further along the road you come to a speed restriction which slows you down, then a red light and finally a large stop sign. Your journey comes to an end and you can no longer travel on that particular road.


Within this story…
- The car represents a person living with HIV
- The petrol represents the medicine
- The bumpy road with different obstacles along the way represents resistance, which stops the car moving as effectively as it should.
So, by taking medicines every day you can continue your journey to wherever you want to go!
Did you know?
Having an undetectable viral load (less than 20 copies/ml) removes the
risk of resistance.
Resistance explained
Drug levels with good adherence
Missed / Late dose
What is sexual health?
Sexual health is something that affects us all. It’s about looking after yourself and others. When we talk about ‘sex’, this includes topics such as being safe, contraception, enjoying healthy relationships, your gender identity, having feelings about another person and being intimate with them.
How do I protect my sexual health?
Consent
It is important that you and your sexual partner do not feel pressured into having sex before you feel ready, and that you both give your consent (permission). There are a number of factors that can affect your ability to consent, such as being under the influence of drugs and alcohol.
Contraception
There are lots of different types of contraception, e.g. the pill, coil, implant, patch or injection. Your clinic team will help you make decisions about the best contraception that will work alongside your current medicines.
Talk to someone
There’s no such thing as a silly question when thinking about sexual health and it’s okay to ask! You are welcome to talk about this in confidence with your clinic team.
Condoms
Condoms reduce the risk of getting or passing on a Sexually Transmitted Infection (STI) and getting pregnant.
Medicines
As you will know, taking your HIV medicines reduces your viral load and therefore
the risk of passing on HIV.
Sexual health screening
This is a check-up of your sexual health. Your clinic team can arrange this or you can visit a sexual health centre (see list of websites) to arrange your own appointment or find drop in times.
Did you know?
It is important to have a sexual health check with each new sexual partner.
Did you know?
You may need a double dose of emergency contraception with your HIV medicine.
Did you know?
Ask your clinic team for further details about accessing free condoms.
Sexual Health Services
Sexually transmitted infections (STI’s) are infections that can be passed from one person to another person during sexual activity. Chlamydia, Gonorrhoea, Genital Herpes, Genital Warts, Pubic lice and Syphilis are some of the STI’s you may have heard about.
STI’s can be passed on through all types of sex:
- Vaginal
- Anal
- Oral sex
STI’s can be spread through any contact with the penis, vagina, anus or mouth – even if there is no penetration. STI’s can affect anyone who is having sex whether you’re straight, gay, lesbian or bisexual.
What do I need to look out for?
Some people may have very obvious symptoms which could include:
- Rashes and itches around the vagina, penis or anus
- Lumps, sores and growths around the vagina, penis, anus or mouth
- A smelly or unusual discharge from the penis or vagina
- Pain when going to the toilet
- Pain when having sex
Some STI’s may have no symptoms at all but can cause damage to our bodies.
How do I get tested and treated?
Many STI’s are curable and all are treatable – so if you think you have an infection or you have had unprotected sex (sex without using a condom), talk to us in clinic or visit one of your local and confidential sexual health services.
Did you know?
70% of females with Chlamydia experience no symptoms at all.
What is PEPSE?
Post Exposure Prophylaxis after Sexual Exposure (PEPSE) is anti HIV medicine that can be given to a HIV negative partner to prevent transmission following a risky situation. E.g. if a condom breaks or you have forgotten to use one.
The risk of passing HIV to your partner is much lower if you are on anti HIV medicines and your virus is undetectable. Should a condom break, you are both protected but it is still important to think about STI’s, which may increase the risk of transmission in this situation.
What do I have to do if a condom breaks, slips off or I have forgotten to use one?
- Tell your partner you have HIV. This can be difficult and your clinic team will be able to
help. There is also advice and guidance in this booklet on the page titled ‘how do I talk
to people about living with HIV?’. - Your partner will need to attend your local sexual health centre.
- The quicker you follow this advice the better! We recommend you seek advice ASAP
and no later than 3 days after sex. - Should your partner need PEPSE, they will have to take this medicine for four weeks.
- If you are undetectable refer to U = U information
There is also PrEP (Pre exposure prophylaxis).
PrEP is medicine taken by a person who is HIV negative. It is taken before and after sex to reduce the risk of HIV transmission. Taking PrEP before being exposed to HIV means the medicine can block HIV if it gets inside the body.
PrEP is available free on the NHS. If you or a partner would like to know more information please ask your clinic staff or your local sexual health clinic.
Back to topHIV transmission covered in law
If you practice safe sex (as described on page titled ‘What is sexual health?’) then you are not breaking any laws. However, unfortunately, some people have gone to prison because of something called ‘reckless transmission’. This is when a person living with HIV has knowingly not protected their sexual partner and transmission has occurred.
The law is only broken if all of these points apply:
- You know you have HIV
- You know how HIV is transmitted
- The person you have sex with doesn’t know that you have HIV
- You have sex without a condom
- You pass HIV on to the person you had sex with
For up to date information on transmission and the law and reckless transmission visit:
www.aidsmap.com and the Chiva website: www.chiva.org.uk/hiv-information/my-rights-2/
U=U (Undetectable=Untransmittable)
U=U means you are taking antiretroviral medicines and you have an undetectable viral load. Therefore, you haven’t missed any doses of your medicines and your HIV has been under control for more than 6 months.
Recent research (The PARTNER Study, 2016) explored 58,000 instances of sex without a condom between partners (one partner Living with HIV, one partner HIV negative). You may be encouraged to learn that results showed that when the Living with HIV partner had an undetectable viral load, there were zero cases of HIV transmission.
What does it mean for you?
You may find it useful to chat further about U=U with your clinic team or visit the Chiva website for more information – www.chiva.org.uk/hiv-information/passing-on-hiv/
Back to topReproductive health – Can I have children?
Absolutely! HIV should not stop you achieving your life goals. You can have a family and importantly, you are very likely to be able to have a child who doesn’t have HIV.
When you’re living with HIV you can have a child with a negative partner without transmitting HIV. Your clinic team can help you with options when considering having a baby.
Taking medication is vital to having healthy children and being a healthy parent.
Did you know?
There are specialist HIV health professionals who can support you and your partner throughout pregnancy.
Did you know?
Every year in the UK many babies are born to women who know they are Living with HIV and almost all of these babies do not have HIV.
Did you know?
Your baby will be closely monitored once it is born. Usually by the time they are aged 3 – 4 months and after three negative blood tests, we are confident that they will be HIV negative. Your baby will continue to be monitored until they are 18 months old.
What is stigma?
Stigma is the strong feelings we have about someone, something or ourselves. Often stigma occurs when people make a judgment based on beliefs, wrong information and misunderstandings rather than knowing the true facts. Unfortunately, there can be a stigma towards people with certain health conditions, including those living with HIV. For example, some may assume that they will get HIV through touch, sharing cutlery and using the same toilet seat, even though we know this is incorrect.
Did you know?
Sometimes people wrongly assume that people living with HIV are to blame for their condition, however, HIV does not discriminate it can affect us all.
What is confidentiality?
Confidentiality is the right for information about you to be kept private. We all have information that we would not want other people to know about without giving our informed consent (permission) first. Informed consent means that you have been informed of the potential implications of giving permission.
When talking to a GP about your health, for example, the information you provide is private and must be kept confidential, unless you have given informed consent for it to be shared, or if the GP has serious concerns that mean confidentiality can be breached.
Did you know?
It is your decision who you chose to share information about your diagnosis with.
Did you know?
The Data Protection Act (1998) is a law to protect your personal medical information.
How do I talk to people about living with HIV?
It can be difficult to share personal health information with others, even more so when there is a stigma attached to a health condition. Sometimes people choose to talk to a family member or a close friend they can trust, although it can be difficult to work out who to tell, how to start a conversation with them and what their reaction will be.
Here are some helpful questions to consider before talking to others about living with HIV:
Who?
- Who would you like to know about your diagnosis?
- Are they close to you?
- Are they trustworthy?
Why?
- Why do you want to tell that person?
- Does telling them help you?
What?
- What will you say to that person?
When?
- When would be the best time to talk?
How?
- How and where will you start the conversation?
Tricky things about sharing your diagnosis
- Once personal information is shared it can’t be taken back
- Some people experience worry or feelings of stress about sharing information
- Sometimes people can react negatively and this can be difficult
- Telling your school/ college or work can be daunting even though there are laws to protect our confidentiality
It can be a relief to share with someone you trust
- You may feel more supported and less alone
- You may feel reassured with the positive experiences of sharing your diagnosis
- You can share responsibility of transmission with your partner
Some top tips
It is important to remember that you have the right to decide who knows about your HIV, as it is your private information.
Young people have said that close friends and family members who know they live with HIV still treat them the same and can provide emotional relief and support when needed.
If you decide to tell someone about your HIV you will need to plan it carefully. Think about what you might say to questions they may have and be prepared for different reactions.
For more information on talking to people about living with HIV visit the Chiva website: www.chiva.org.uk/infoyp/talking-about-hiv
Did you know?
To prepare for a conversation, it can help to think about how you felt when you were told you were living with HIV and the different questions you had.
Did you know?
Your employer usually won’t need to know your status. However, you could choose to tell them if you feel it would benefit you.
Did you know?
You can practice having a conversation about sharing information with a member of your clinic team.
What jobs can I do?
There are thousands of job options and almost all of these are open to you. Like anybody else, the biggest challenge for you will be getting the qualifications, skills and experience you need.
If you are interested in doing so, you can work in the medical profession as a doctor, nurse, midwife etc. as long as you look after yourself and maintain an undetectable viral load if undertaking invasive procedures.
Do employers need to know my diagnosis?
In most cases the answer to this question is no. You won’t have to tell them but you may choose to tell them.
The law says that:
- Employers must keep your personal information private
- Employers cannot discriminate against you because of your status
- The Equality Act 2010 protects everybody from discrimination due to things like age, race, sex or disability. HIV is covered within this act.
Some top tips
- It’s your choice who you tell
- Plan what you will say first
- Sharing information can be a positive experience
Useful links for further information:
- www.aidsmap.com/about-hiv/do-you-have-disclose-your-hiv-status-employer
- www.aidsmap.com/about-hiv/do-i-have-tell-anyone-i-have-hiv
- www.nat.org.uk/nat-topic/rights-equality-and-discrimination
Can I go on school trips, sleepovers & parties?
Of course you can! An important part of your life is joining in with a range of different activities, including travel, trips and social events.
It can sometimes be difficult to remember to take your medicines when you’re not in your usual routine or when you are among people who do not know about your medicines.
Here are some top tips:
- Plan what you might say if people ask you about your medicines.
- If your school knows you are living with HIV discuss your medicines with the member of staff you know and trust.
- If your school does not know you may decide it is time to tell them and you can read more about this on the page titled ‘How do I talk to people about living with HIV?’. You can also always talk to your clinic team.
- It is a good idea to have a trusted adult who can remind you to take your medicine and have somewhere to store it safely.
- If you decide not to tell and you are able to manage your own medicines, the clinic team can offer suggestions about the best way of doing this.
- A text message from your parent/family member or alarm on your phone can help remind you about taking your medicine while you’re away.
- Remember to plan it all in plenty of time, it helps to be organised. Please get in touch with your clinic team if your medicines are running low.
- See Chiva website for more information www.chiva.org.uk/travel
Did you know?
You can use an unmarked pill box or container in your toiletry bag.
Did you know?
It is okay to say that your medicines are a daily vitamin tablet that lots of people
need to take.
What is a healthy lifestyle?
We all have to think about our physical and our emotional health. Here are some top tips and ideas about how you can look after yourself.
Exercise
We all need to exercise. The National Health Service (NHS) suggests we should try to exercise every day for 30 minutes or more. This can include having a fast walk, going for a jog, a swim, dancing, karate, bike riding, playing football, the list is endless! Basically, anything that gets you working hard enough to raise your heart rate and break a sweat.
Doing this is excellent for:
- Improving heart function
- Maintaining a healthy weight
- Improving bone health
- Improving mental health
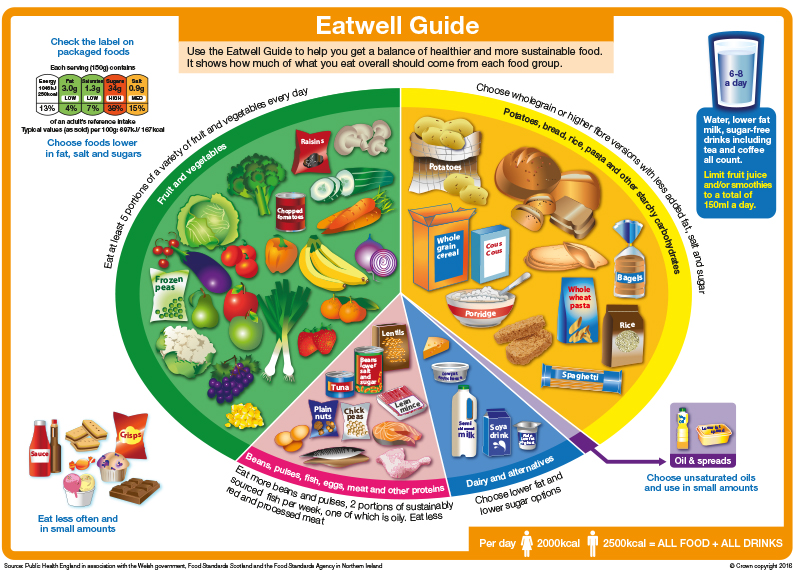
Diet
Being mindful of what we choose to eat and drink can have an impact on our weight, health, energy levels, concentration and mood. The Eatwell Guide on the next page is a useful tool to check that you are eating a balanced diet.
- Fruit and vegetables: Which 5 portions of fruits and vegetables do you enjoy?
- Proteins: How would you include some protein in your diet?
- Dairy: Do you include dairy in your diet?
- Carbohydrates: Do you get enough variety of carbohydrates?
- Water: Do you drink enough water?
- Do you ever check your food labels for fat, salt and sugar content?
Did you know?
Exercise can also help to improve your self confidence and allow
you to develop new social skills.
Did you know?
Scientists have discovered that exercise makes your brain release chemicals that make you feel good!
Did you know?
Calcium is important for growing bones and teeth. To absorb calcium from our diets we need vitamin D. The majority of vitamin D in our bodies comes from sunlight. Vitamin D levels frequently drop particularly during winter months. Your clinic team can provide a practical guide on increasing your calcium/vitamin D.
Alcohol and Drugs
We know that misusing alcohol and drugs can poison the human body and affect our physical and emotional health. We would encourage you to talk openly with your clinic team about any experiences with alcohol and drugs, as these may cause interactions with your medicines. Also, this allows us to support you. Here’s what some young people said about alcohol and drugs…
“When you are under the influence of drugs and/or alcohol, you are very vulnerable”
“Personal problems can’t be fixed with drugs and/or alcohol”
“If friends are drinking and using drugs and you don’t want to join in you can say no”
“It is important to talk to people you can trust about any pressures to drink or try drugs”
Did you know?
Some over the counter medicines, gym supplements and herbal remedies can interact with your medication. Always speak to your clinic staff before starting any.
Did you know?
You can speak to your clinic team in confidence if you are concerned
about alcohol and / or drugs affecting you or your family/ friends.
Emotional well-being
We all have difficult thoughts and feelings from time to time and it can be a really unsettling and isolating experience. We know that talking to a person you can trust can be really helpful, here are some ideas why:
‘It was a relief to share how I was feeling, like a weight had been lifted’
‘I felt listened to and like my worries were important’
‘There will always be challenges in life; sometimes we can’t tackle them alone and need help.’
‘Talking things through felt comforting’
‘I was able to look at my problems more clearly’
‘My problems seemed smaller once they were out in the open’
‘I felt reassured knowing that everyone goes through challenges in their lives’
‘Together we found new ideas to stop me feeling stuck.’
‘I was supported and knew someone cared about me.’
‘I learned new techniques to help me’
‘I found strengths I didn’t realise I had’
Top tips for emotional wellbeing
It is usually best if you can talk to someone you trust about how you feel. However, it is not always easy to start conversations and there are lots of other things that may help you with your thoughts and feelings, here are some top tips:
- Express yourself through art and creativity
- Play sport, dance, exercise – anything that makes you feel good
- Write your thoughts and feelings down
- Make time to relax and unwind
- Remember the things you are great at, all those talents, skills and qualities
Where can I get help?
Clinic Team
Some services have access to Psychologists, who are there to listen and assist you with your physical and emotional health. Your clinic team will be able to guide you in finding a professional to help you. You can also talk to your GP about local support services.
School / College
If you feel able, you can talk to staff, such as a mentor, head of year or school counsellor.
Where else can I get help?
Childline
0800 1111 – A free, confidential phone line for young people, where trained counsellors are available to support you anytime day or night. You can also contact and chat to a counsellor online via https://www.childline.org.uk
Samaritans
116 123 – A free, confidential, phone line for adults open 24 hours a day, 365 days a year. You can also email [email protected]
Did you know?
It is very common to experience emotional difficulties. It is estimated that 1 in 4 people living in the UK have or are experiencing mental health problems.
Did you know?
We know that our emotional health is as important as our physical health.
Travel
Travelling can be an exciting adventure, which allows you to gain new experiences. When planning a trip abroad, there are a few things to consider that will help you enjoy your trip and stay safe. It is always important to plan trips with as much notice as possible to allow for HIV medicines to be supplied to cover the duration, and to receive all the appropriate vaccinations and malaria tablets if required. Some HIV medicines increase sun sensitivity, so it is important to practise sun safety including using sunscreen, seeking shade, and covering up with clothes and a hat.
Can I work abroad?
Yes you can! People living with HIV can live and work in most countries. Lots of countries have no restrictions, however, there are a few small exceptions.
For information on travelling, living or working abroad, as well as health advice and travel vaccines visit:
- www.chiva.org.uk/professionals/clinical-guidelines/
- www.nhs.uk/using-the-nhs/healthcare-abroad/apply-for-a-free-uk-global-health-insurance-card-ghic/
- www.fitfortravel.nhs.uk
- www.hivtravel.org
- www.tht.org.uk/hiv-and-sexual-health/living-well-hiv/your-rights/travelling-hiv
- Or call THT direct on 0808 802 1221 to speak to an advisor
Did you know?
Did you know, you must always buy travel insurance when traveling abroad.
This allows you to access care and treatment abroad.
Did you know?
Availability of anti-retroviral medicines varies from country to country.
Did you know?
You can take condoms to any country. It’s a good idea to plan ahead
and be prepared.
Groups and Peer Support
Meeting other young people living with HIV
At first it may seem daunting to think about meeting other young people living with HIV or joining a support group. This is understandable and it is normal to feel apprehensive meeting others and trying something new. However, like lots of things, once you make that first step it can open up lots of opportunity to meet others, talk about living with HIV openly in a safe and confidential environment, try new experiences, gain new skills and importantly, have fun!
Here are some quotes from young people who attend one support group in Leeds called ‘Together 4 Life’
“The reason why I started the group was to make friends. At first I was scared and shy but when I got there they were really friendly and nice and everyone welcomed me.”
“If you are part of the group you are part of a big family, they are always there for you. Skyline made me grow up and start thinking about my health.”
“During the group I have made new friends that I know will be there for a long time. They have made me feel comfortable. I am able to trust the people within the group and I know I can trust them with my heart. I can now walk with my head held high.”
“The group has really given me support. They have made a confident bright person I am today. They have been there through good and bad times. I really enjoy going to the group. I have developed a lot more knowledge than before.”
Ask your clinic team about HIV support groups in your area.
As well as local services, there is a national organisation, Chiva, who provide lots of helpful information and support, including peer mentoring, for young people living with HIV. In 2010 Chiva set up ‘Freedom To Be’ a yearly support camp for young people living with HIV. At camp, you are able to join in creative workshops, try exciting outdoor activities and express yourself, whilst having fun and building friendships.
“As long as I try I can do anything” (Young person after attending Chiva camp 2017)
Back to topWhat is transition?
In healthcare, we use the word “transition” to describe the process of preparing, planning and moving from children’s services to adult services.
Transition is a gradual process that gives you, and everyone involved in your care time to get you ready to move to adult services and discuss what healthcare needs you will require as an adult.
Transition is about making plans with you – and not about you.
We understand that moving away from your team can sometimes feel scary but we hope that this pack and ongoing discussions with your team will help you feel more confident and happier about the move.
Age 12+
Build my health knowledge. Start talking about transition.
Age 13-15
Continue to build my health knowledge. Introduce Ready, Steady, Go! Increasing my independence.
Age 15-16
Getting ready to move to young adult services.
Age 16-18
Welcome to your Adult Clinic
Read a young person’s transition story on the Chiva website:
www.chiva.org.uk/hiv-information/transition-story/
Transition Packs
In clinic we may go through a transition pack e.g. ‘Ready Steady Go’ with you at each visit. This is a really useful guide in getting you thinking about moving on and feeling prepared for adult services. There are different transition plans depending on which clinic you attend. Please discuss with your clinic team.
Back to topYour Paediatric Team
Throughout your time in clinic you will meet different members of your paediatric team. You can use your printed booklet to write down their names and contact details.
Back to topYour Adult Team
Throughout your time in clinic you will meet different members of your adult team. You can use your printed booklet to write down their names and contact details.
Back to topWhat young people attending clinic in Leeds have to say about transition
“It’s another step towards a long journey. Just know you are not alone and there are others in your position.” Written by B.S
“Transitioning is like moving forward. Think of it as a journey, just like when you have to move from year 7 to year 8 in school. At first it will all seem scary but remember you are definitely not alone.” Written by T.D
“You are not alone. There is always someone to talk to.” Written by N.S
“There is always someone to talk to, you are not alone. You will always feel welcome and there is support for you anytime of the day.” Written by B.S
“Personally, I treat the transition as if it was like moving from primary to High school. There isn’t much difference other than the maturity that is required for a successful transition.” Written by N.S
Back to topCommunication in clinic
You can use the table provided in your printed booklet to help with discussions between you and your clinic staff. We have suggested some topics to help communication but there are also spaces at the bottom for topics you would like to bring up.
Back to topWelcome to your adult clinic!
When you and your clinic team feel you are ready, you can move on to your adult clinic. Talk to your clinic team about having a look around beforehand so that you are familiar with how to get there, the reception area, waiting area and clinic rooms. If you haven’t already done so, you can also start to get to know the team.
Back to topUseful Resources
Websites for advice, support and information
- www.chiva.org.uk – Chiva, National
- www.4mmm.org – 4M Mentor Mothers Network, National
- www.blueskytrust.org – Blue Sky Trust, North East & Cumbria
- www.brigstowe.org – Brigstowe Project, Bristol area (18+)
- www.ght.org.uk – George House Trust, Manchester
- www.kpsdirect.com – Kernow Positive Support, Cornwall
- www.thebha.org.uk/locations/leeds – Leeds Skyline, Leeds
- www.positivelyuk.org – Positively UK, National
- www.positiveeast.org.uk – Positive East, London
- www.positivehelpedinburgh.co.uk – Positive Help, The Lothians, Scotland
- www.sahir.org.uk – Sahir House, Merseyside
- www.tht.org.uk – Terrence Higgins Trust (THT), National
- www.sussexbeacon.org.uk – The Sussex Beacon, Sussex
- www.foodchain.org.uk – The Food Chain, London
- www.waverleycare.org – Waverly Care, Scotland
Acknowledgements
We would like to thank the following people and organisations for their contributions and support with this project:
- Young people and families within the Paediatric HIV Service at Leeds Teaching Hospitals NHS Trust
- The Paediatric and Adult HIV Teams within the Leeds Teaching Hospitals NHS Trust
- Sian Shenton, Pharmacist for Leeds Children’s Hospital
- Gilead for kindly part funding this project
- Dr Chetcuti, Consultant Paediatrician at Leeds Teaching Hospitals NHS Trust, for kindly part funding this project
- Chiva and additional charities and organisations who support young people to live well with HIV
Contact details
We would love to receive any comments/feedback in relation to the pack. Please send to: