Introduction
What is TAVI?
Transcatheter Aortic Valve Implantation (TAVI) is a treatment for disease of the aortic heart valve. It was developed as an alternative to open heart surgery and involves putting a new heart valve in place using a less invasive (‘keyhole’) approach.
It is most commonly performed under local anaesthetic through an artery in the top of the leg, but in a small number of cases a general anaesthetic or incision in the chest wall may be needed.
The world’s first TAVI procedure was performed in 2002, and the first procedure in Leeds in 2008. The procedure is now being performed increasingly frequently and several million patients have been treated worldwide. Leeds is one of the most experienced TAVI centres in the UK.
This leaflet will provide you with information about the TAVI procedure itself, as well as what to expect before and after TAVI. If you have any questions, then please do not hesitate to discuss them with a member of the TAVI team.
Why might I need TAVI?
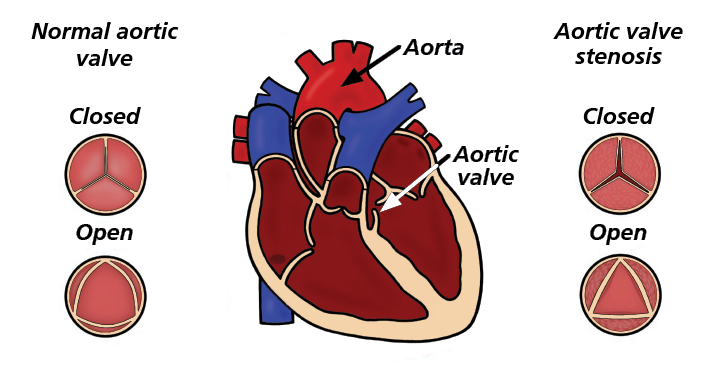
As the heart muscle contracts to pump blood around the body, the blood passes out of the heart through the aortic valve. This valve opens to allow the blood to flow out, then closes to prevent blood flowing back in the wrong direction. As people get older, the aortic valve can degenerate and become either narrowed or leaky.
These problems can cause symptoms including breathlessness, chest pain, dizziness, blackouts, or ankle swelling. As well as affecting quality of life, they can also reduce life expectancy if left untreated.
TAVI is most commonly used to treat severe narrowing of the aortic valve (known as aortic stenosis). It can sometimes be used to treat severe leaking of the aortic valve (known as aortic regurgitation), or degeneration of a previous tissue aortic valve replacement.
For many years doctors have treated aortic valve disease by replacing the aortic valve using open-heart surgery. This is a well-established and very effective operation. However, in some patients, such as older patients, those with other medical problems, or those who have had previous cardiac surgery, the risks of surgical aortic valve replacement are higher. TAVI allows the aortic valve to be replaced without the need for open heart surgery, and therefore is a good option for some patients in whom the risks of surgery are unacceptably high.
Aortic valve stenosis
Is TAVI right for me?
What are the benefits?
In patients who are selected for TAVI, there is a very high chance (more than 95%) that the valve can be successfully replaced and the new valve functions well.
After a successful procedure your symptoms will usually be considerably improved. In most patient’s symptoms of breathlessness, chest pain, dizziness and blackouts are either abolished completely or are only mild after the procedure. This typically results in a considerable improvement in exercise capacity and quality of life.
What are the risks?
Although TAVI does not involve open heart surgery, it is still a major procedure and carries some risks. This is partly because of the procedure itself, and also because patients undergoing the procedure are often older people and/or have other medical problems.
The risks are different for each person, and the team will discuss the risks with you before you decide to go ahead with the procedure.
Typical risks from TAVI include:
- 2% risk of not surviving the procedure to leave the hospital;
- 2% risk of a major stroke, and 3% risk of milder stroke;
- 10-20% chance of needing a permanent pacemaker;
- 5% risk of significant bleeding or vascular complication requiring intervention (such as blood transfusion or an operation);
- 5% risk of moderate-severe leaking of the TAVI valve;
- 2% risk of infection of the heart valve; less than 1% risk of serious kidney damage, allergic reaction, heart attack, or need for urgent open heart surgery.
It is important to bear in mind that the risks associated with the TAVI procedure itself are usually outweighed by the risk of leaving the underlying aortic valve disease untreated.
More than 90% of patients report feeling significantly better after their TAVI procedure. However, a small number of patients report that they feel little difference after an apparently successful TAVI. The reasons for this might be that the original symptoms were provoked by a co-existent problem such as severe lung disease or frailty. Part of our assessment is to identify these factors and advise patients on our expectation of symptom improvement.
What are the alternatives?
The team will discuss the alternative treatment options with you before you decide to have a TAVI.
These options may include:
- Surgical aortic valve replacement: Open heart surgery is a well-established and very effective treatment. It carries a higher risk in some patients but may be preferable to TAVI in other patients.
- Balloon Aortic Valvuloplasty: This uses a balloon to temporarily stretch open the narrowed aortic valve. It may be used in carefully selected patients but is generally not a long-term solution.
- Medication: Drug treatment can sometimes help to improve symptoms, but it cannot address the underlying narrowing of the valve, and the effectiveness of drug treatment alone is limited. Without a procedure to relieve the narrowed valve, symptoms are likely to persist and deteriorate and life-expectancy may be reduced.
The Leeds TAVI information film
The TAVI team at Leeds have produced a short information film about the TAVI pathway and procedure. It provides a great deal of information about what to expect and a chance to hear from patients who have undergone the procedure, as well as members of the TAVI team. Most patients find this useful in helping them to understand more about the procedure and answer questions that they may have. We recommend that all patients (and their loved ones) watch the film as part of the preparation for considering TAVI.
You can search this on YouTube channel and is entitled:
The TAVI Journey – A Patient’s Perspective.
It can also be accessed through this link:
https://www.youtube.com/watch?v=3aPLVGYGdkU.
We can also provide a DVD or can be watched at the preassessment visit.
Back to topWhat are the steps in the TAVI assessment pathway?
What tests will I need?
In order for us to assess your suitability for this procedure we will provisionally arrange a number of investigations once we have received your referral.
Nearly all patients will need to have:
- Outpatient appointment with consultant cardiologist (in some cases you may be asked to see a cardiac surgeon as well). You may also meet the Valve Nurse Specialist at this appointment. The consultation will provide us with information about your symptoms, lifestyle, physical and mental health as well as frailty. Please note that age is not an excluding factor.
- Transthoracic echocardiogram: This provides information about the heart and valve using ultrasound. This may be repeated in Leeds even if you have had one performed previously in your local hospital.
- TAVI CT angiogram: This is a sophisticated x-ray providing detailed 3-dimensional pictures of the aortic valve, heart arteries, and the other blood vessels throughout the body. You will receive an injection of a special dye so that the blood vessels and heart structures show up clearly. This test is needed to assess whether the anatomy is suitable for TAVI, to determine the size and type of TAVI valve, and assess the best access route to use for the procedure.
- Electrocardiogram (ECG): This places stickers on the chest to record the heart rhythm and electrical activity of the heart.
- Blood tests: Blood is taken to measure your blood count and kidney function.
Other tests that are sometimes required.
Some patients may require additional tests. These may include:
- TAVI angiogram: This x-ray study gives us information about the heart arteries and the femoral arteries. A slim tube is inserted through an artery in your groin or wrist and guided to the heart. A special dye is injected through the tube to show the arteries clearly.
- Trans-oesophageal echo: Ultrasound images of the heart are taken with a probe placed inside your oesophagus, providing a more detailed assessment of the heart valves.
- Stress echocardiogram: Ultrasound images are taken while the heart rate is deliberately increased (either with exercise or drugs) to assess the severity of the aortic valve disease and the contraction of the heart muscle.
- Lung function test: This measures lung capacity and how well the lungs are working.
Not all of the listed tests will be required. We will determine which tests will be appropriate in your case. You may have already had some tests carried out, in which case we will review the results of these. However, please note that you may need some tests repeating.
You will receive these appointments through the post. Where possible we do try to limit the number of visits to hospital. Therefore, you may need to spend approximately 4-6 hours when you come to your clinic appointment as we will aim to perform most of the tests on the day.
Valve MDT Meeting
After your screening tests have been completed and you have been seen in the clinic by your consultant your case will then be discussed in a multi-disciplinary team (MDT) meeting made up of relevant valve specialists, including consultant cardiologists, consultant cardiac surgeons, imaging specialists, TAVI nurse specialists, and sometimes others (such as vascular surgeons or anaesthetists).
We will analyse all of the data and information to make an informed decision about the best management and treatment option for your condition.
What are the possible outcomes from the valve MDT meeting?
Once your case has been discussed we will try and contact you via telephone to inform you of the decision. You will also receive written confirmation.
The common outcomes are:
- Accepted for TAVI: Your name will be added to the waiting list for the TAVI procedure. The waiting times vary and your TAVI specialist nurse will be able to give you an approximate time.
- Recommended for open heart surgery: You and your GP will be informed of the decision and the process that follows.
- Recommended for treatment by Balloon Aortic Valvuloplasty: This is a treatment in which we stretch open the aortic valve using a balloon. The benefits are only temporary, and this is only usually done in certain situations.
- We may recommend no intervention: This is when we feel that the valve disease is not severe, treatment is not appropriate or possible, or the risk of TAVI outweighs any benefit.
Dental care before your TAVI
It is essential to maintain healthy gums and teeth especially if you have heart valve disease. This is to reduce the risk of dangerous infection of the heart valves, known as endocarditis.
It is important that you have dental checks before your heart valve procedure. It may be recommended that dental treatment is necessary, and this may need to be carried out before TAVI is performed.
Please register to a dental practice if you do not see a dentist regularly. Simply find a dental practice that’s convenient for you, whether near your home or work, and phone them to see if there are any appointments available.
If you are unable to find dental practice accepting NHS patients, you should call NHS England’s Customer Contact Centre on 0300 311 2233.
Back to topThe TAVI procedure
The pre-assessment visit
Once you have been allocated a date for your procedure you will be invited to attend a pre-assessment clinic, so we can review your health and discuss your admission.
You will see the Valve Nurse Specialist at this appointment and will have the opportunity to ask questions regarding your procedure, your hospital stay, rehabilitation and recovery. You may wish to bring a friend or family member with you during this visit.
If you are taking anticoagulation tablets (such as warfarin, apixaban, rivaroxaban, dabigatran, or edoxaban) you will be given instructions about when to stop these before the procedure.
While you are waiting for your hospital admission, it is important to contact the Valve Nurse Specialist should your symptoms worsen or your health start to deteriorate. We will also need to be informed of any unplanned admissions to hospital. The contact number is 0113 392 5298.
What does the procedure involve?
TAVI is usually performed under local anaesthetic with some sedation. You will be lying flat and will be awake, but relaxed, during the procedure. Sometimes it may be performed under a general anaesthetic, if required.
In most cases the TAVI valve is inserted through the femoral artery, which is accessed through a small incision at the top of the leg. This is known as the transfemoral approach. We use this approach whenever possible (in 90-95% of cases). The procedure usually takes 1-2 hours.
When the transfemoral approach cannot be used, an alternative approach will be adopted, most commonly through an incision under the collarbone (using the axillary or subclavian artery). The team will explain which approach they plan to use for you.
A wire is placed through the aortic valve and a long tube (known as the ‘delivery sheath’) is then passed over the wire. The delivery sheath contains the new valve, which is a ‘tissue valve’, made out of material from a cow or pig’s heart sewn into a metal frame. The delivery sheath is positioned across the aortic valve, and the valve is then deployed. The metal frame containing the valve expands, pushing your old valve out of the way, and allowing the new valve to start working immediately. The delivery system is removed, and the artery closed using a special closure device. There are usually a few stitches in the skin.
A number of different TAVI valve devices are used, selecting the option that is best suited to your individual needs.
Is the TAVI procedure painful?
Most patients are nervous about the procedure. You will feel pressure and a some stretching sensation when the delivery tube is inserted into the artery in the groin. This is briefly uncomfortable. At the end of the procedure this tube is removed with similar sensation. The valve implant itself is not painful but you may feel light-headed as we deliberately lower the blood pressure for a few seconds.
You will always have a trained nurse or anaesthetist monitoring you carefully, and strong painkillers or sedatives are sometimes needed to help keep you comfortable. Most patients report that it was not as bad as they were expecting.
Back to topCare after the TAVI procedure
When can I go home?
This will be decided once the procedure is finished. You will usually be discharged home either the following day, or the 2nd day after the procedure. Sometimes it is necessary to stay in for a few days longer. Where possible, we recommend that a relative or friend drives you home or accompanies you.
After the TAVI procedure most patients go to Ward L20 (LGI Jubilee Wing F-floor) or Ward L14 (LGI Jubilee Wing E-floor). You will be attached to a heart monitor and have regular checks of the access site. You will have to lie flat for several hours after the procedure.
The visiting times for these wards vary. It is best to contact the wards directly for visiting times. Contact details can be found on your admission letter.
Groin care after transfemoral TAVI
It is normal for the groin site to be tender and bruised for a few days after the procedure.
Seek medical attention if you notice any of the following:
- A persistent hard, tender lump under the skin
- Increased pain, swelling, redness or discharge at the groin site
- A cold and pale hand or foot on the same side as the procedure
- Raised temperature or fever.
In the unlikely event that your groin starts to bleed you should lie down. Apply pressure to the area keeping your or leg (or arm, if the incision was made here) as straight as possible. If bleeding does not stop after 10 minutes you must seek immediate medical attention at your local A&E department.
It is preferable to shower rather than have a bath for the first week, until the wound is healed.
It is important to remember you will have stitches in your groin and these should be removed after 5-7 days – please contact your practice nurse about this.
Wound care after subclavian/axillary TAVI
Your dressing should be removed before you go home. If the wound is clean and dry, you need not have the wound redressed.
You may have some stitches which are dissolvable and therefore do not need removing.
Please look at your wound daily in a mirror. During working hours please report any extra swelling, redness, oozing, hotness to touch and/or excessive pain to the TAVI nurse on 0113 392 5298. Out of hours you should contact your GP or local A&E department.
What follow-up will I have?
You will be followed up in the outpatient clinic by the Valve Nurse Specialist approximately 6-8 weeks after your TAVI procedure.
We will arrange for you to have a transthoracic echocardiogram on the same day as your outpatient appointment.
After your first follow up, you will need an annual check-up with echocardiogram to monitor the heart valve function. We will arrange this if you live in Leeds and will ask your local cardiologists to arrange annual follow up if you are not from Leeds.
Some patients need to have a 24hour ECG monitor fitted once you are back at home. We will assess if this is necessary before your hospital discharge. For non-Leeds patients this can usually be done at your local hospital.
Back to topRecovery after TAVI
How long will I take to recover?
Time taken to completely recover will vary from patient to patient. On average it will be at least 1-2 weeks for recovery from the procedure. Some patients will take longer and some less.
Will my medication change?
Your medication is very likely to change, and the ward staff will take you through all of your medicines before your discharge. Many patients will be advised to take Aspirin (or an equivalent drug such as Clopidogrel) life long, unless you are already on an anticoagulant (such as warfarin, apixaban, rivaroxaban, dabigatran or edoxaban).
If you have any queries about your medication, please contact your GP or the Valve Nurse Specialist.
What physical activity can I do?
It is important that you re-introduce exercise gradually after discharge from hospital.
You could start with everyday activities such as walking around the house and climbing stairs, building up your activities gradually.
1st week
Take things slowly and rest if you need to.
You should avoid:
- Lifting, pulling and pushing anything heavy
- Housework such as cleaning or vacuuming
- Gardening
After the first week:
Aim to gradually increase exercise by walking only. More vigorous exercise than walking should be left for at least four weeks after the procedure.
Walking programme instructions
Start at Stage 1 of the walking guidelines and remain at each stage for at least two consecutive days or up to several days depending on how you feel.
Only move onto the next stage when you feel comfortable with the current stage. As you progress it may take longer before you move onto the next stage.
If you are unwell, do not do the activity. You may need to drop back a stage or two when you feel well enough to resume the activity.
| Stage | Time in minutes | Times per day | Pace |
| 1 | 5 | 1-2 | Stroll |
| 2 | 10-15 | 2 | Comfortable |
| 3 | 15-20 | 2 | Comfortable |
| 4 | 20-25 | 1-2 | Comfortable/stride out |
| 5 | 25-30 | 1-2 | Comfortable/stride out |
| 6 | 30+ | 1-2 | Comfortable/stride out |
Warm-up and cool-down
It is very important that you include a warm-up and a cool-down into your activity. The warm-up prepares the body for the activity ahead.
It should be a gradual build-up of movements before you start the main part of your programme. It will increase your heart rate and breathing rate.
The cool down should be a gradual decrease of movement at the end of your activity. It will bring down your heart rate and breathing rate and return.
When can I drive?
DVLA guidance requires that you do not drive for 4 weeks after TAVI. You do not need to inform the DVLA about your procedure, unless you hold an HGV / bus license. We do advise you to tell your insurance company to avoid problems with any claims you make in the future.
If you have problems with your insurance the British Heart Foundation (BHF) will be able to give you details of insurance companies on 0845 070 8070.
If you hold a commercial licence you will need to inform the DVLA who will advise you further.
Drivers Medical Group, DVLA, Swansea, SA99 1TU,
Tel: 0300 790 6806
Back to topOther frequently asked questions
When can I fly or travel abroad?
We generally advise not to fly for four weeks after the TAVI procedure. You may want to discuss with the TAVI team before you make any plans to travel abroad.
Holiday insurance can sometimes be a problem and some airline companies may ask for a medical certificate to say that you are medically fit to fly.
You must inform your holiday insurance company, or you may not be covered.
When can I return to work?
This will depend on many factors, such as the overall state of your health and the type of work that you do. Please discuss this with your TAVI nurse specialists or doctor.
Emotions after TAVI
Having a TAVI is a significant life event, and may affect you emotionally, as well as physically. Moods and feelings may be change rapidly, and you may feel low in mood or tearful at times. This is a normal part of recovery and these feelings will pass. If you experience any problems either physically or emotionally post-procedure it is important to mention these to your GP so that he/she can monitor them and help with your symptoms.
Dental Care after TAVI
We recommend regular dental check-ups after TAVI to reduce the risk of infection which can be serious if it spreads to the heart valve.
Antibiotics may be recommended for some treatments – you should inform your dentist that you have had a TAVI and they will discuss this with you, if required.
Back to topResearch
Leeds is one of the largest TAVI centres in the UK and we are actively involved in a large number of national and international research studies related to TAVI. Some of these studies involve investigating the very latest valves or devices that may potentially help to reduce the chances of complications, while others involve the comparison of different established treatments.
Some studies do not involve new treatments but involve an extra investigation so that we can better assess the benefit of the TAVI treatment.
You may be invited to participate in one of these studies. If you are, then the purpose of the study, and what is involved, will be explained to you in detail. You are, of course, entirely free to decline to take part in any study and your treatment will not be affected in any way.
Back to topContact details
Valve Nurse Specialist
Tel: 0113 392 5298
Email: [email protected]
Ward L20 Tel: 0113 392 7420
Ward L14 Tel: 0113 392 7414
Cardiology bed manager Tel: 07825 028 321
Back to topAdditional information and support
British Heart Foundation
The website contains a wealth of helpful information on all aspects of heart disease including the conditions, tests, treatments, and rehabilitation.
Tel: 02079 350 185
Helpline: 0300 300 3311
Email: [email protected]
Website: www.bhf.org.uk
Heart Valve Voice
This charity provides information and support for people with heart valve disease.
Tel: 07399 606 386
Email: [email protected]
Website: www.heartvalvevoice.com
Valve for Life UK
An initiative aims to improve and expand access to life-saving and life-changing minimally invasive ‘key-hole’ therapies for heart valve disease across the National Health Service.
Tel: 01455 552 559
Email: [email protected]
Website: www.valveforlife.co.uk
Back to topContributors
The contents of this book were developed by: Dr Michael Cunnington, Consultant Cardiologist and Kerry Pena, Cardiac Valve Nurse Specialist.