This leaflet aims to help you and your family understand more about your Total Body Irradiation treatment.
It is given to you in addition to the information you will receive from your Clinical Oncologist (who is a specialist doctor in cancer treatment). Their team will be caring for you during your treatment. This team includes doctors, physicists and radiographers.
The leaflet describes the radiotherapy test dose and treatment. It also explains the side-effects which you may experience during and after treatment.
Each person’s treatment will vary, so the information given is a general guide. The healthcare team looking after you will explain your treatment and the side-effects in detail.
If you have any questions after reading this leaflet, please speak to the team looking after you or ring the numbers at the end of leaflet. Staff will make every effort to meet your individual needs or will direct you to the person who can help.
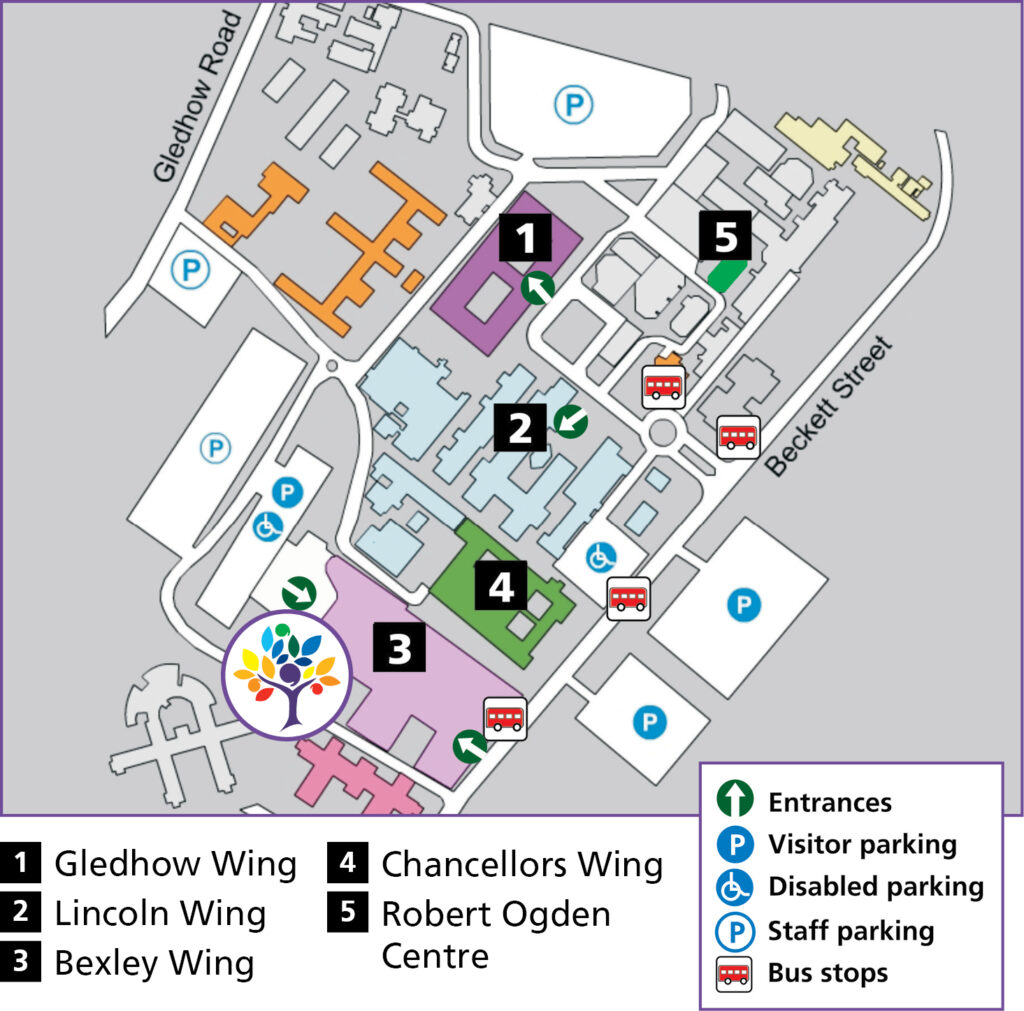
All your radiotherapy planning and treatment will take place in the Radiotherapy Department on Level -2, Bexley Wing, Leeds Cancer Centre (LS9 7TF).
Radiotherapy reception Tel: 0113 206 8940
Please do not bring any valuables into hospital with you as the Trust cannot accept liability for loss or theft.
What is Radiotherapy and Total Body Irradiation (TBI)?
Radiotherapy is the use of high energy X-rays to treat cancer. TBI is a type of radiotherapy used to prepare you for a stem cell or bone marrow transplant (BMT). It is given in combination with chemotherapy to kill any remaining cancer cells and help your body to accept the donor marrow.
Some transplant types will only require a single radiotherapy treatment whereas others may require up to eight treatment visits.
The tissues of the body are made up of tiny building blocks called cells. The radiotherapy causes damage to cancer cells in the treated area. Although normal cells are also affected, they can repair themselves and are able to recover. During total body irradiation all the cells in your body receive a dose of radiotherapy but most will recover in the weeks following treatment. Side-effects will be explained further on in this leaflet.
When you are having your radiotherapy you do not feel anything and it does not make you radioactive. You may hear a buzzing noise when the machine is switched on.
You will have your radiotherapy on a treatment machine called a Linear Accelerator as shown here.

Who will I meet?
Clinical Oncologist
This is a specialist doctor in cancer treatment. He or she will be responsible for consent review and prescribing your course of radiotherapy.
Therapeutic Radiographers
Radiotherapy is given by therapeutic radiographers of any gender, who are highly trained in the accurate planning and delivery of radiotherapy treatment. You will see your radiographers at your test dose and each treatment session, and they will be happy to answer any questions you may have.
Radiotherapy Physicists
Radiotherapy physicists work with the other members of the team to plan your radiotherapy treatment. They perform calculations to make sure that you receive the correct dose of radiation.
Student therapeutic radiographers
The radiotherapy department is a training centre for therapeutic radiographers. They are supervised at all times. If you do not wish students to be present, please speak to a member of staff. This will not affect your treatment or care.
Others involved in your care
You may meet other staff whilst you are coming for radiotherapy.
Everyone you meet will introduce themselves, tell you their job title and explain the role they have in your care.
Pregnancy
It is very important that patients of child-bearing potential are not pregnant at the start of a course of radiotherapy and that they do not become pregnant during a course of radiotherapy because it can have an effect on the unborn child. Use an effective form of contraception, for example condoms, coil, depo injection or contraceptive pill.
For more information see the ‘Contraception and pregnancy during cancer treatment’ leaflet. Please do not hesitate to ask your doctor or nurse if you have any questions or concerns about these issues.
Planning your treatment
Before your TBI you will have an appointment to see the clinical oncologist in the haematology department on Level 3, Bexley Wing. You will be given an appointment to attend the radiotherapy department for a ‘test dose’. These may be separate appointments, or combined in one visit and will usually be about two weeks before your radiotherapy treatment.
When you see the clinical oncologist, he or she will explain the test dose and treatment, any possible side-effects and answer any questions that you might have. It is a good idea to make a list of any questions before you attend for this appointment.
Why do I need a test dose of TBI?
We use the test dose to plan your TBI treatment. You will receive a very small dose of radiotherapy at this appointment which will not cause you any after effects.
The dose of radiotherapy across your body will be carefully recorded and measurements are used to produce an individual treatment plan for you.
The test dose uses exactly the same process as for your TBI treatment, except that the dose of radiotherapy given is very much smaller.
What happens at the test dose?
There will be several staff in the treatment room with you at first, they are radiographers and radiotherapy physicists.
They will help you to get into the right position in a large, mouldable bean bag for your test dose.
Once you are in the correct position, you will have small sensors taped to various parts of your body to measure the dose of radiation to each area. A perspex (thick clear plastic) screen will be placed between you and the treatment machine.

Both the radiographers and radiotherapy physicist will leave the room to switch on the machine. You will only be alone for a few moments at a time. The radiographers will be watching you on a Closed Circuit TV monitor (CCTV) to make sure you are alright. The CCTV camera is not recording or saving any images.
There is also an intercom system so the radiographers can talk to you. If you would like to listen to music during your treatment, please let us know.
You will receive half of the test dose facing the radiotherapy machine. The radiographers will then come into the room to turn the couch around and the other half of the test dose will be given with your back to the machine. The treatment machine will only be switched on for 1-2 minutes in total.
It makes a buzzing sound when switched on. You do not feel anything. This whole procedure takes about 20-30 minutes in total, and you will be fine to go home as soon as it is finished.
What position will I be in for the TBI?
You will lie on your side in a ‘bean bag’ on an adjustable couch, which is four metres away from the treatment machine. A perspex screen will be placed in front of the couch during treatment.

This is to make sure that your whole body receives the right dose of radiation. The screen and the radiotherapy machine will not touch you.
What should I wear?
It is helpful if you can wear trousers without any metal such as leggings or tracksuit bottoms, and a tight fitting T-shirt. This will avoid the need to undress completely.
How is TBI given?
You will be an inpatient for your TBI treatment, staying in a side room on the Haematology ward. You will have between one and eight treatments depending on your diagnosis and the type of transplant you will have.
Treatment will be twice a day if you are having more than one treatment.

Each treatment lasts about half an hour. Most of this time is spent making sure that you and the treatment machine are in the right position for the treatment. The radiotherapy machine will be on for about ten to fifteen minutes of this time.
We have a wide selection of music available to play during treatment; please let us know if you have a particular preference.
During the TBI you are in the same position as you were for the Test Dose. During some treatments the sensors may be used again to check the dose of radiation.
If you are receiving eight treatments, after the fourth treatment you will be asked to lie on the opposite side for your remaining appointments and the bean bag will be re-moulded around you. This will be done in the treatment room during your appointment.
Will I feel ill during or after the TBI?
You will be given an anti-sickness injection through your Hickman line before each radiotherapy treatment. If you still feel sick after the treatment, please tell the nurses on the ward.
Side-effects
Side-effects can be divided into short term (acute) effects, that happen during or soon after treatment, and long term effects occurring months or years later. Some side-effects are common, whilst others are rare. Your oncologist will discuss this with you. If you develop any radiotherapy side-effects you will be given advice and support by your healthcare team.
Short term side-effects
The possible side-effects listed below are much less likely for people having only one or two TBI treatments. Your clinical oncologists will talk about your individual risk of developing side-effects. This will depend on the type of transplant that is planned.
The side-effects of TBI may include:
- Redness or darkening of the skin which settles about two to three weeks after your radiotherapy has finished.
- Swelling of the salivary glands which settles within days after your radiotherapy has finished.
- Soreness of the mouth, throat and difficulty in swallowing. This usually lasts two to three weeks. You will be given pain relief as needed.
- Diarrhoea – This lasts about three to five days and starts after the radiotherapy has finished. You will be given anti- diarrhoea capsules.
- Tiredness and sleepiness – Radiotherapy can make you feel more tired than usual. Be prepared to take things easy during treatment and allow for extra rests. There is a Macmillan information leaflet on fatigue. If you would like a copy or support with your fatigue please ask a member of staff.
Fatigue usually improves several weeks after treatment.
There are things you can do to help yourself:
Gentle exercise can help reduce the symptoms of fatigue.- Having enough to drink can prevent tiredness from dehydration.
- Small meals or snacks eaten more than three times a day may be easier to face.
- Try to get a good night’s sleep where possible.
- Try to ‘pace’ yourself and listen to what your body is telling you. Rest if you need to.
- Pick out the things that you enjoy and try to accept help with other tasks.
- Little and often is the rule of thumb.
- Veno-occlusive disease – Very rarely a condition, called veno-occlusive disease, can develop where the small veins of the liver become inflamed. This is a serious problem that can affect how the liver works. You will be monitored for any early signs of this.
Long term side-effects
Eyes
The commonest long term side-effect of TBI is cataracts. Your vision will be checked regularly in an outpatient clinic. If you do develop cataracts these can be treated with surgery.
Hormones
TBI, like chemotherapy, affects the cells of the ovaries or testes and usually results in infertility. Early menopause may also develop. TBI may result in low levels of other hormones such as thyroid hormone many years after treatment. This can be corrected with tablets.
Lungs
Pneumonitis is inflammation of lung tissue and can develop in a small number of people six weeks to six months following TBI. This can cause shortness of breath or cough.
Heart
Radiation to the heart can increase the long term risk of heart disease such as heart attacks many years after TBI. To reduce other risks of heart disease, it is important to follow a healthy lifestyle.
For example:
- Taking regular exercise,
- eating a balanced diet, and
- not smoking.
Brain
TBI can occasionally have a subtle effect on higher mental function (how your brain works) some years after radiotherapy. An example of this could be developing problems in short term memory.
Other Cancers
The radiotherapy from TBI can result in a small risk of developing other cancers. The risk is very small compared to the potential benefit of treatment. Please discuss this with your consultant. You will be advised not to smoke and to protect your skin from the sun in the future to minimise this risk. Women will also be advised on screening for breast cancer.
Further information and support
If you have any questions please ask your hospital team. We all have our own ways of coping with difficulties.
Some people have a close network of family and friends who provide emotional support. Others would rather seek help from people who are not involved with their illness.
The following are also available as sources of information and support that you may wish to use.
Clinical Nurse Specialists (CNS)
Your CNS is available to discuss any aspect of your treatment with you. You will be seen by a CNS before your treatment. This is to offer support and advice about the practicalities and effects of your treatment and answer any questions you may want to ask.
Your CNS will also assess and discuss any physical, psychological, social, occupational and spiritual needs that you may have. They can refer you to other services if needed, for instance, benefits advice.
You should be given a ‘key worker’ as a contact for support through your treatment; this is usually your CNS.
Macmillan Specialist Radiographer and Macmillan Radiotherapy Nurse Specialist
Sometimes people need more help if they are feeling depressed, very anxious or are having problems with their treatment. If this is the case you may benefit from seeing the Macmillan radiographer or nurse specialist.
Your oncologist, radiographer or nurse can refer you at any point before or during your treatment.
Local Support Services
Leeds Cancer Support
Leeds Cancer Support complements care provided by your clinical team. We offer access to information and a wide range of support, in a welcoming environment for you, your family and friends.
We can be found in the information lounges in Bexley Wing and also in the purpose built Sir Robert Ogden Macmillan Centre (behind the Thackray Medical Museum).
The Sir Robert Ogden Macmillan Centre
This centre offers a variety of free health & wellbeing and supportive therapies for patients, their family members and carers. These include hypnotherapy, mindfulness coaching, acupuncture (for hot flushes) and pilates.
Contact numbers for Leeds Cancer Support
Information Lounge Level -2 Radiotherapy Department
Open from 8.00am – 6.00pm Tel: (0113) 206 7603
Information Centre Level 1 Outpatients Department
Open from 9.00am – 4.00pm. Tel: (0113) 206 8816
Sir Robert Ogden Macmillan Centre
Open from 9.00am – 4.00pm. Tel: (0113) 206 6498
All the above services can be emailed on:
[email protected]
Maggie’s Centre
If you or someone you love has cancer you may have lots of questions. Maggie’s is a warm, welcoming place where you can meet people who are experiencing similar things to you.
You may also be able to find support groups specific to your needs and get advice and information from their professional staff.
You don’t need an appointment and all support is free.
Open Monday to Friday 9.00 am – 5.00pm. Tel: 0113 457 8364
Address: St James’s Hospital (next to the multi storey car park), Alma Street, Leeds LS9 7BE
Email: [email protected]
Website: www.maggies.org
National Support Organisations
Macmillan Cancer Support
Freephone: 0808 808 0000, 8am to 8pm seven days a week.
A textphone service for deaf and hard of hearing people on 18001 0808 808 0000 Website: www.macmillan.org.uk
Stopping smoking
NHS Free Smoking Helpline: 0300 123 1044 Monday to Friday 9am to 8pm, Saturday and Sunday 11am to 4pm.
Website: www.nhs.uk/smokefree
Cancer Research UK
Website: www.cancerresearchuk.org
Live Through This
A cancer support and advocacy charity for the LGBTIQ+ community.
Email: [email protected]
Website: https://livethroughthis.co.uk
Car Parking
When you are coming for radiotherapy planning and treatment your parking is free in the on-site multi-storey car park. Please ask for more information at the radiotherapy main reception desk.
Refreshments
There is a restaurant and coffee shop available on Level 0, which are open daily. They serve drinks, light snacks and hot meals. Vending machines are also available in the main radiotherapy waiting room and Level 0. There is also a shop on Level 0 with books, papers and snacks.
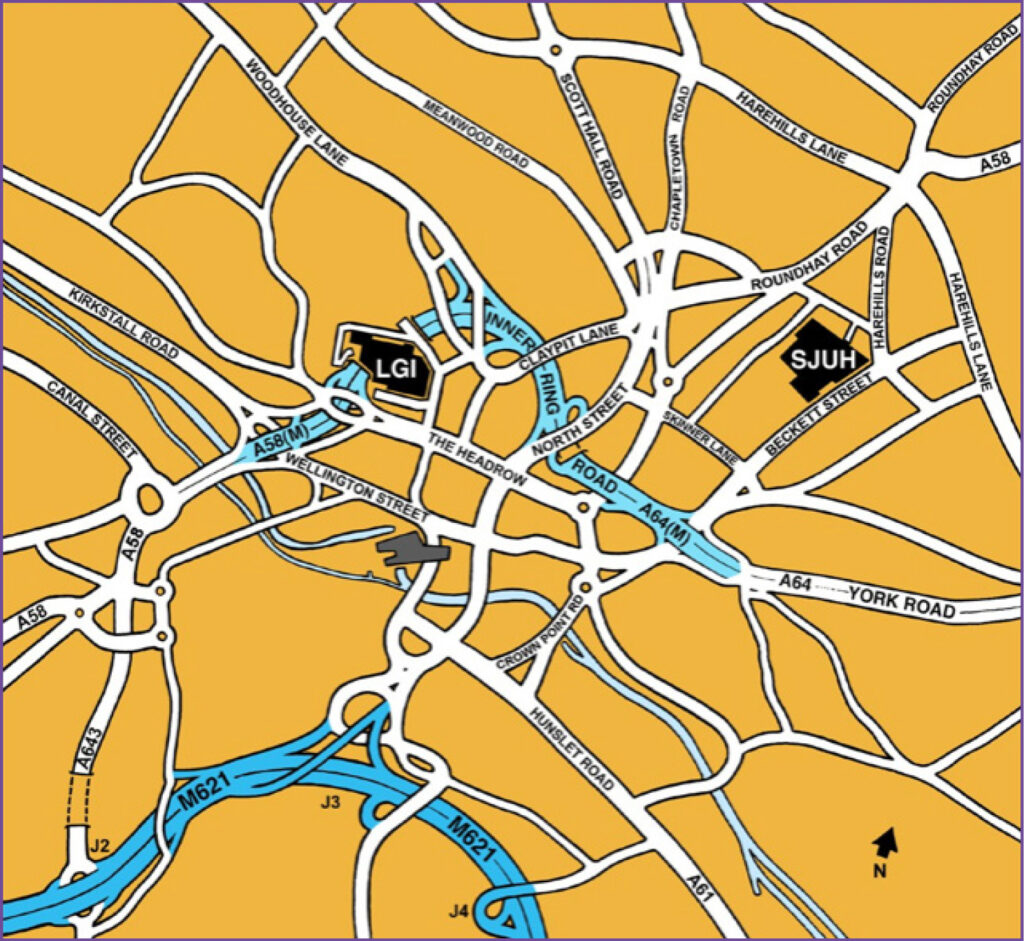
How to find us

This leaflet is under review and has been approved for a temporary print run from 09/10/2024 MIS:20241007_009/EP