This booklet has been written to answer some of the questions you may have about your surgery for ovarian mass or suspected ovarian cancer.
You will be given a separate leaflet called ‘Gynaecological Oncology Surgery – Enhanced Recovery Programme’ which will explain about what to expect when you come in for your surgery and advice for recovery at home.
Diagnosis
Your doctor may have told you that you have an ovarian mass, tumour or cyst on one or both of your ovaries.
Your doctor may have said that they are concerned about the results of your investigations and that you need surgery to see if there is any cancer present.
In most cases, a diagnosis of ovarian cancer cannot be made until after your operation.
Why not confirm the presence of ovarian cancer before undergoing surgery?
The only way to confirm the presence of cancer within the ovary without an operation is to take a biopsy from it.
This requires inserting a needle into it to retrieve tissue for examination under the microscope, but may cause leaking of cancer outside the ovary if it was malignant (cancerous) which could then spread to other areas of your abdomen. Therefore the safest way to take a biopsy is with surgery to remove the mass.

What are the ovaries?
The ovaries are part of a woman’s reproductive system. There are two ovaries, the size and shape of almonds, one on either side of the womb. In women still having periods (pre-menopausal), the ovaries produce hormones and eggs. Menopause happens when the ovaries stop producing the hormones necessary for the menstrual cycle and periods.
What are the fallopian tubes?
The fallopian tubes receive eggs produced by the ovaries and carry them to the inside of the womb.
What is the peritoneum?
The peritoneum is a continuous membrane which lines the abdominal cavity and covers the abdominal organs providing separation and support.
What is an ovarian or fallopian tube mass?
An ovarian or fallopian tube mass (can also be called a pelvic mass) is mostly identified through the use of scans such as ultrasound but in some cases can also be felt as a lump by yourself or by a healthcare professional.
There are several causes of pelvic masses, some of which are non-cancerous (benign) and some cancerous (malignant).
Borderline ovarian tumours are not cancerous and are treated by surgery. Some masses are found to be borderline ovarian tumours. 95% of these tumours are cured by surgery alone but due to a small risk of recurrence, you may require follow up for a few years. Your consultant will discuss this with you if your tumour is found to be borderline in nature.
Non-cancerous pelvic masses may occur due to infection, endometriosis and fibroids amongst other reasons.
Cancerous masses usually arise in the ovaries but can also originate from the fallopian tubes or peritoneum.
There are different subtypes of ovarian cancers that affect women of different ages and have different prognosis and treatment. Your doctor will discuss the type of tumour suspected in your case.
Surgical options
Why is surgery performed?
Surgery may be recommended because your symptoms, background history, scans and blood tests are associated with an increased risk of your pelvic mass being cancerous.
Your case will have been reviewed at our multidisciplinary team (MDT) meeting which involves a range of healthcare professionals who carefully consider your options to identify which one is best for you. These options are then discussed with you.
What are the surgical options?
There are 4 options:
- Gold standard staging laparotomy.
- Removal of the affected ovaries for frozen section and proceed according to the result.
- Two-stage procedure.
- Fertility-sparing procedure.
1. Gold standard staging laparotomy
This operation is recommended in most cases, especially if there is a suspicion of cancer. It is usually performed through a vertical midline cut (incision) in your abdominal wall. This incision allows the surgeon to investigate for any signs of cancer in all areas of your abdomen.
This surgery usually involves removal of the uterus (womb), cervix, fallopian tubes and ovaries, as well as the omentum and lymph nodes in your pelvis and abdomen.
The lymphatic system helps protect us from infection and disease. It is part of the body’s immune system. Lymph fluid passes through lymph nodes. A network of lymph vessels connects the lymph nodes together. You have nodes throughout your body.
The omentum is a fatty pad that is attached to the stomach on one end and part of the bowel on the other. It is partially or completely removed even if it looks normal as it may sometimes contain cancer that is not visible with the naked eye.
In some cases, the surgeon may find cancer deposits on other organs. These may have not been visible on the initial CT scan as they can be very small in size. If this is the case, removing all visible cancer is important. To achieve this, different organs in your abdomen may need to be removed. They may include the spleen, liver surface, appendix or the peritoneum covering the diaphragm (muscle that helps with breathing).
The peritoneum is a smooth lining that covers all the organs inside the abdomen. It is sometimes involved with visible deposits of cancer. Where possible this lining is removed along with the cancer deposits.
This is not always possible without removing the organ covered by the peritoneum.
2. Removal of the affected ovary or ovaries for frozen section and proceed according to the result
Frozen section examination is a test that can be performed if the surgeon finds no obvious evidence of cancer when they look inside your abdomen, at the time of the operation.
Frozen section refers to a microscopic examination of the abnormal mass by a pathologist while you are asleep under anaesthetic in order to see whether there is any evidence of cancer or borderline changes. This type of examination is correct in about 90% of the time.
If a frozen section confirms cancer we proceed to perform gold standard staging laparotomy as in surgical option 1.
The frozen section aims to reduce the risk of lymphoedema (leg swelling) which happens in about 1 out of 10 women that have a pelvic lymphadenectomy (removal of the lymph nodes from the pelvis).
3. Two-stage procedure
This involves having two operations.
At the first operation the suspicious mass is removed and tested for cancer. If a mass is confirmed to be cancer, then we would carry out a staging laparotomy, as in surgical option 1, at a later time
If the ovary removed is proven not to contain cancer, a second operation is not needed.
4. Fertility-sparing procedure
This option is commonly selected for women who wish to have children in the future.
The suspicious ovarian/fallopian tube mass is removed but the other ovary, fallopian tube and uterus remain in place.
The lymph nodes, omentum and peritoneum can be removed as per the gold standard procedure.
This procedure may increase the risk of cancer recurrence if the disease in the ovary is confirmed to be cancer and a second operation may be suggested by your doctor.
What are the risks of surgery?
There are risks associated with any surgical procedure. Your surgeon will explain these risks to you before you sign your consent form. This form confirms that you agree to have the operation and understand what it involves.
Possible risks and complications are:
- Problems caused by having a general anaesthetic; for example, you may feel sick afterwards. It is also possible to have an allergic reaction, although this is rare. Please tell your doctor about any allergies you have.
- Heavy bleeding during or after the operation; this may need to be treated with a blood transfusion.
- Infection; This would be treated with antibiotics.
- Damage to your bowel, bladder or ureters (the tube that carries urine from the kidneys to the bladder) during surgery – this would be repaired during your operation.
- A blood clot in the leg (deep vein thrombosis) which can sometimes lead to a blood clot in the lungs (pulmonary embolus) – moving around as soon as possible after your operation can help to prevent this. You will be given surgical stockings (known as TEDS) to wear and injections to thin the blood which both help to reduce the risk of blood clots. You may continue to have these injections for up to four weeks.

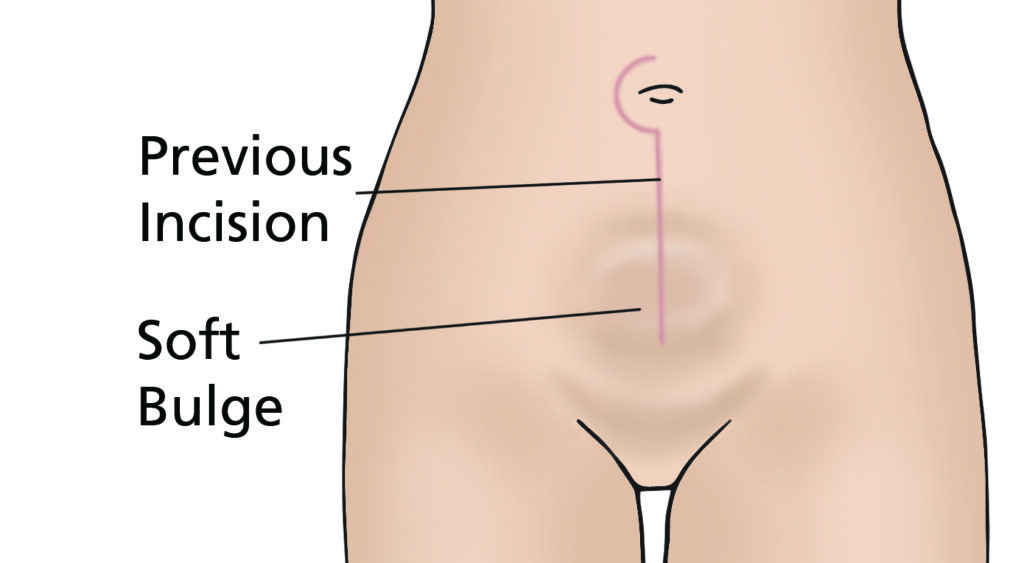
- Incisional hernia; where there is a weakness in the wound allowing tissue or bowel to push through and appear like a bulge. Incisional hernias can develop months or years after surgery and are repaired by another operation.
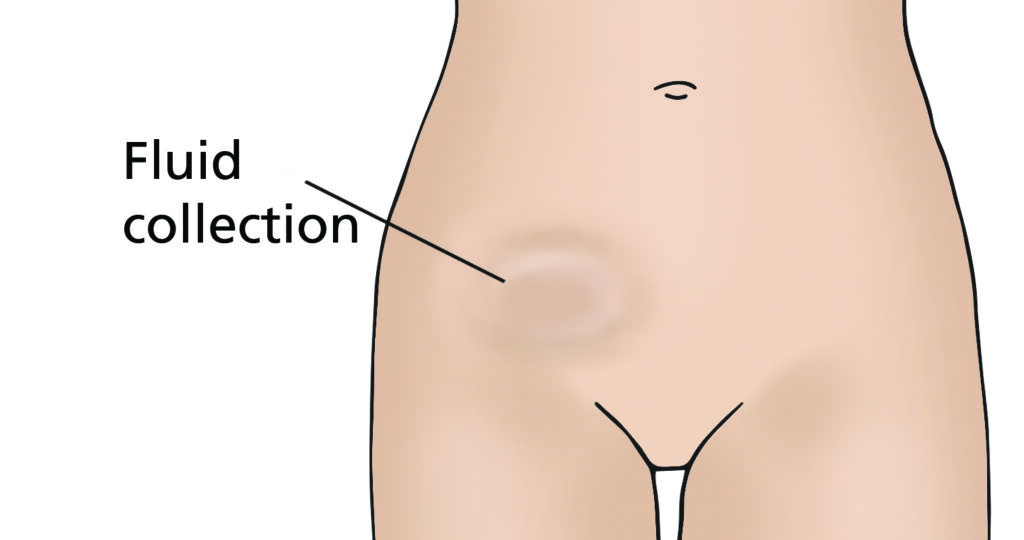
- Lymphocyst; This is a fluid collection at the site where lymph nodes have been removed. The fluid is often naturally reabsorbed by your body but may require draining if large or causing you discomfort.
- Lymphoedema; if you have some lymph nodes removed during surgery there is a small risk that in the future your body will find it harder to drain fluid from your legs and lower body. This causes swelling of the legs and lower body known as lymphoedema. If you develop this problem then you can be treated by a lymphoedema specialist. You can discuss this further with your gynaecology specialist nurse or doctor. There is also a booklet you can read that can give you more information.

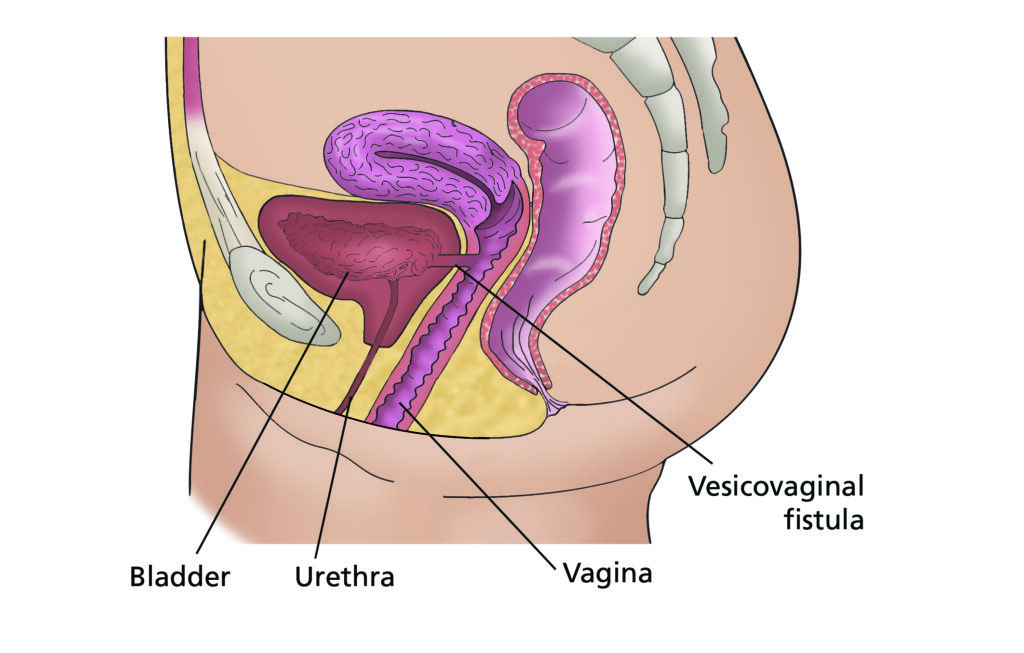
- A vesicovaginal fistula; is a hole between the bladder and vagina. It causes urine to pass from the bladder to the vagina.
- A rectovaginal fistula; is a hole between the rectum and the vagina. It causes faeces to pass from the rectum to the vagina.
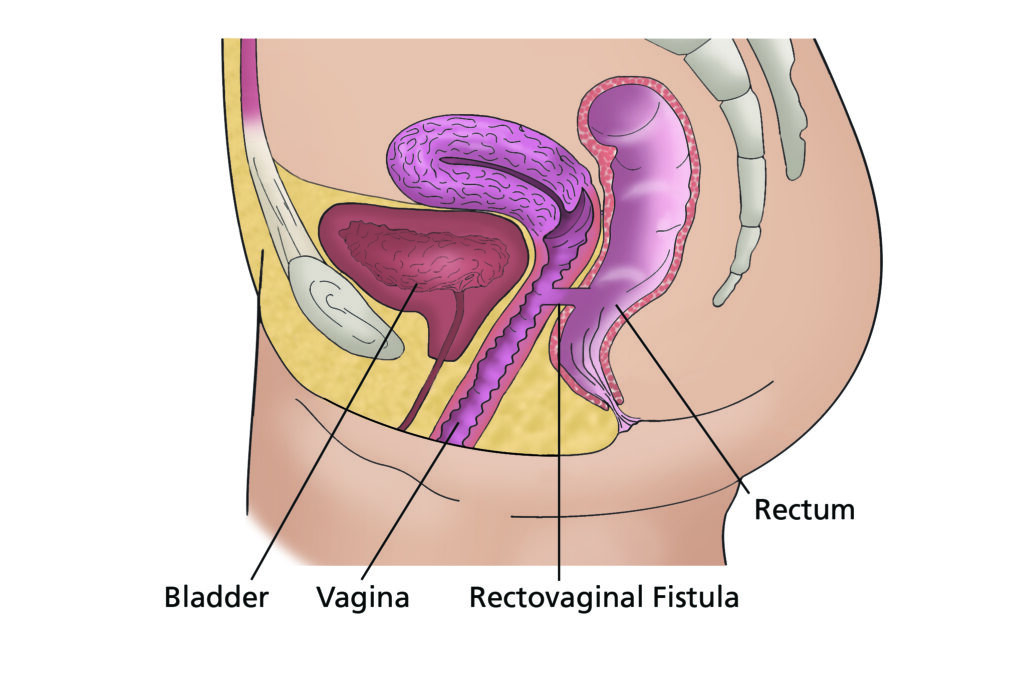
Fistulas can be repaired but sometimes it will involve another operation.
What else might happen as a result of surgery?
Occasionally, depending on the extent and position of the mass, tumour or cyst, the surgeon may have to operate close to, or actually include the bowel. If an area of bowel must be removed, the remaining sections of the unaffected bowel may be joined back together if it is safe to do so. Sometimes it is not safe to join the bowel and so part of the bowel is opened onto the abdominal wall. This is known as a colostomy (if large bowel diverted) or ileostomy (if small bowel diverted). Both are referred to as stomas. The stoma allows the stools (faeces) to be collected in a bag attached to your tummy, which can be removed and emptied. If this is a possibility, it will be explained to you in more detail by your surgeon. A stoma is likely to be permanent but occasionally can be reversed.
Your surgeon may request a colorectal nurse specialist to see you before your operation. The nurse will mark the area of your tummy where a potential stoma could be formed. They will also provide education and emotional support.
If a stoma is formed during your surgery, you will be supported on the ward to help you become confident with caring for your stoma. Once discharged home you will have access to a community stoma nurse specialist team. The possibility of having a stoma can worry many patients. Please talk through your concerns with your surgeon or clinical nurse specialist team, who can support you with any decisions.
Your bladder may take some time to begin working properly again. Some women have a loss of feeling in their bladder and therefore do not know when their bladder is full. This may take some time to return to normal. During this time you need to go to the toilet regularly to empty your bladder.
Some women find that their urine stream is slower so it may take longer to pass urine.
This usually improves as your body recovers from surgery. Rocking gently backwards and forwards or side to side whilst sat on the toilet can help to fully empty your bladder.
Your bowels may take some time to begin working properly again. Some women have a sluggish bowel for a number of days after surgery which can cause you to feel sick until it starts to work again. If this happens then you will be advised to walk around the ward as much as possible to stimulate your bowels to work.
This can be difficult if you are feeling unwell but it is important to do so to help speed up your recovery. We will also give you anti-sickness medication. Passing wind is a good sign that your bowels are starting to work.
Trapped wind and wind pain is very common after surgery. Walking around as much as possible can help relieve this. You may find that peppermint tea and/or peppermint capsules are helpful which are both available on the ward. Wind usually starts to improve once you are having your bowels opened.
What about losing my fertility if I have a hysterectomy?
A number of different factors influence whether or not HRT is recommended. Please speak to your consultant for further information or advice.
Should I continue to have cervical smears?
Cervical smear tests are not necessary if you have a hysterectomy as your cervix will have been removed. If you haven’t had a hysterectomy then you will need to continue to have regular cervical smears.
Is there anything I should do to prepare for the operation?
Make sure that all of your questions have been answered and that you fully understand what is going to happen. You are welcome to visit the ward and meet the staff before you are admitted to hospital – ask your specialist nurse or pre-assessment nurse to arrange this.
You should eat a balanced diet, and if you feel well enough, take some gentle exercise before the operation, as this will also help your recovery afterwards. Your GP, practice nurse or the doctors and nurses at the hospital will be able to give you further advice about this.
Before you come into hospital for your operation, try to organise things for when you come home. If you have a freezer, stock it with easy to prepare food.
Arrange for relatives and friends to do your heavy work (such as changing your bedding, vacuuming and gardening) and to look after your children, or other dependants if necessary. Arrange for somebody to take you home from hospital when you are discharged. If you think you may have problems managing at home, you can discuss this with the nurses on the ward.
Is it normal to feel emotional or low in mood after my operation?
Yes. It is a very common reaction to the operation. If these feelings persist when you leave the hospital, you may wish to discuss them with your GP or specialist nurse.
There are also local and national support groups that you can contact. Details are given at the end of this booklet.
When can I go home?
You will usually be able to go home around 4-5 days after your operation. This depends on your individual recovery, how you feel physically and emotionally and the support available at home. If you require hospital transport for your discharge home, please let a member of staff know well in advance.
Will I need to visit the hospital again after my operation?
Yes. It is very important that you attend any further appointments arranged for you, whether this is at your local hospital or in Leeds. The tissue results (histology) from your operation can take around 3 weeks.
An appointment for the outpatient clinic will be made to discuss these results with you and if any further treatment is necessary. We will refer you to a medical oncologist if you need chemotherapy.
Please visit our website where you will find patient information leaflets and videos related to your surgery
Useful Numbers
For queries regarding your admission please call the relevant secretary.
Contacts
For advice please call your Clinical Nurse Specialist (CNS) or Ward J98
If your nurse specialist is not available then please leave a message on the answering machine and they will ring you back. Please note this may not always be the same day.
In an EMERGENCY please attend your nearest Accident and Emergency Department.
Local Support Services
Leeds Cancer Support
Leeds Cancer Support complements care provided by your clinical team. We offer access to information and a wide range of support, in a welcoming environment for you, your family and friends.
We can be found in the information lounges in Bexley Wing and also in the purpose built Sir Robert Ogden Macmillan Centre (behind the Thackray Medical Museum).
The Sir Robert Ogden Macmillan Centre
This centre offers a variety of free health & wellbeing and supportive therapies for patients, their family members and carers. These include hypnotherapy, mindfulness coaching, acupuncture (for hot flushes) and pilates.
Contact numbers for Leeds Cancer Support
Maggie’s Centre
If you or someone you love has cancer you may have lots of questions. Maggie’s is a warm, welcoming place where you can meet people who are experiencing similar things to you.
You may also be able to find support groups specific to your needs and get advice and information from their professional staff. You don’t need an appointment and all support is free.