Molar Pregnancy and Gestational Trophoblastic Neoplasia are two uncommon conditions where a pregnancy does not develop normally. Together they are called Gestational Trophoblastic Disease.
The purpose of this information leaflet is to explain:
- What a molar pregnancy is.
- What gestational trophoblastic neoplasia is.
- What the treatment options are.
- What the follow-up involves and why it is important.
- What things you may want to consider after you have received treatment for molar pregnancy or gestational trophoblastic neoplasia.
What happens in the development of a normal pregnancy?
An (embryo) baby develops when a sperm fertilises an egg.
The genetic material from each combines to produce a baby which has half its chromosomes (genetic material) from each parent.
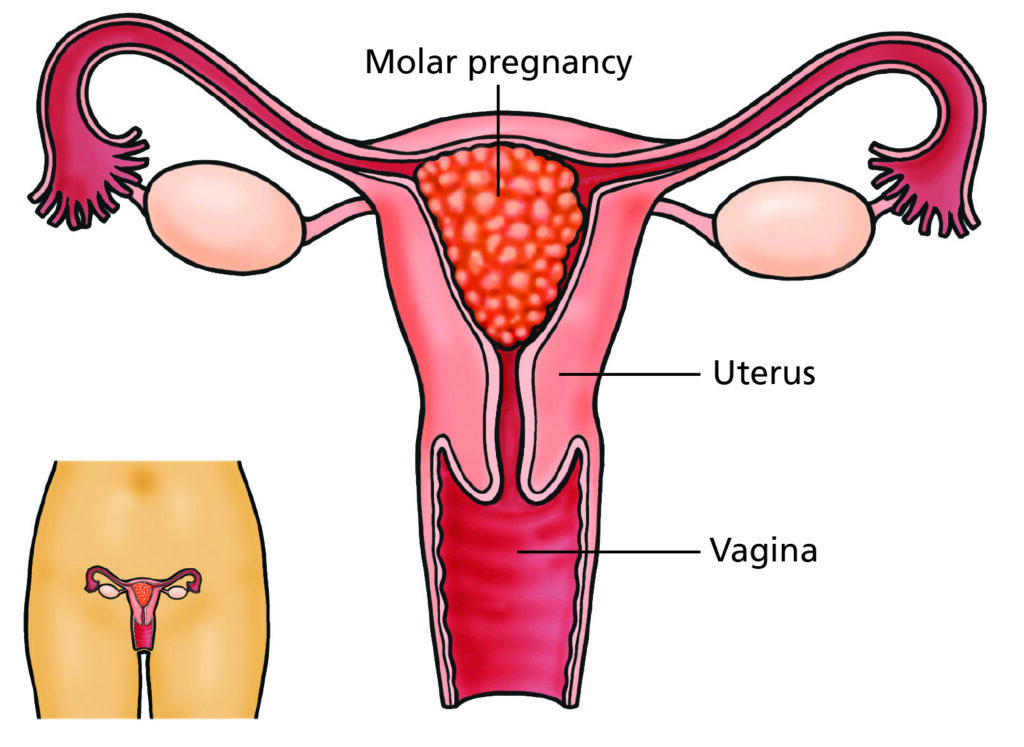
What is a molar pregnancy?
A molar pregnancy is when a pregnancy is developing abnormally. It is sometimes called a hydatidiform mole. It occurs in less than 1 in 700 pregnancies.
It is abnormal from the very moment it is formed. It is the result of an imbalance in the number of chromosomes supplied from the sperm and from the egg. It cannot develop into a fully developed baby. You cannot do anything specific to reduce your chance of having a molar pregnancy.
There are two types of molar pregnancy:
Complete molar pregnancy
- In this type of pregnancy there is no developing baby.
- A complete molar pregnancy normally happens because
a single sperm has fertilised an ‘empty’ egg (an egg
which has no chromosomes in it). The sperm’s
chromosomes duplicate in the egg so that there are
two sets of chromosomes which both come from the sperm. - A complete molar pregnancy can also happen when
two sperm fertilise an ‘empty’ egg.
Partial molar pregnancy
- This type of pregnancy, two sperm fertilise a chromosomally normal egg. This means that there are three sets of chromosomes in the pregnancy. Two are from the sperm and one is from the egg.
- In some cases of a partial mole there can be early signs of a baby on ultrasound scan, however, the pregnancy is always chromosomally abnormal and cannot survive.
Very rarely
There can be a twin pregnancy where one twin is a molar. If this is suspected you will be referred to a specialist centre.
Why does a molar pregnancy happen?
A molar pregnancy normally happens by chance. However, there are risk factors.
These include:
- Being under 20 years old.
- Being over the age of 40.
- Having had a molar pregnancy in the past.
- Being of Asian (Indian, Pakistani, Bangladeshi) origin.
What symptoms can you get with a molar pregnancy?
You might have no symptoms associated with a molar pregnancy. However, if you do have symptoms they might include:
- Missed period and a strong positive pregnancy test.
- A lot of nausea (feeling sick) or vomiting.
- Irregular bleeding from the vagina.
- Symptoms similar to those experienced in a miscarriage.
How is a molar pregnancy diagnosed?
- Pelvic ultrasound Scan
Complete molar pregnancies can be strongly suspected on an ultrasound scan because they have a particular appearance on scan. Partial molar pregnancies are more likely to be diagnosed after a pregnancy loss when the cells of the pregnancy tissue is tested (see below). - Test of pregnancy tissue (Histology)
The only definite way to diagnose a molar pregnancy is to examine the pregnancy tissue in a laboratory. Most molar pregnancies are diagnosed in this way after you have had surgical treatment for miscarriage. At the end of the procedure the pregnancy tissue that has been removed is sent to be examined with your permission.
Please note
It may take several weeks for these results to be processed. If molar pregancy is diagnosed you will be informed.
How is a molar pregnancy treated?
You will be offered treatment if you have a definite or suspected molar pregnancy.
There are two ways to treat a molar pregnancy. Your doctor will discuss them with you and may recommend one over the other. These options include:
- Medical management
- Surgical management
Surgical management
This is the preferred choice of treatment in most molar pregnancies. If your doctor suspects that you have a complete molar pregnancy you will be offered surgery. This is usually done under general anaesthetic (put to sleep). The pregnancy tissue is removed from your uterus and sent to the pathology laboratory to check the diagnosis. You are normally able to go home the same day but may need to stay overnight.
Medical management
Medical treatment is not an option if you have a suspected complete molar pregnancy. You may be offered medical management if have a partial molar pregnancy.
Medication is given (either by mouth or into the vagina) to cause the molar pregnancy to miscarry (to come away). You may need to stay in hospital until you have passed the pregnancy tissue. The pregnancy tissue is then collected and sent to the pathology laboratory to check the diagnosis.
Anti-D
You only need anti-D if your blood group is rhesus negative and you receive surgical management of your suspected molar pregnancy.
Registration with a centre specialising in Gestational Trophoblastic Disease
If you are confirmed to have a molar pregnancy or gestational trophoblastic neoplasia, we recommend that you are entered into a specialist follow up programme. The doctor will ask you if your personal details can be registered with a specialist centre. This is so that your treatment can be coordinated and provided by doctors who are experts in this field.
There are three such centres in the UK. The nearest one for our local population is the Trophoblastic Screening and Treatment Centre in Weston Park Hospital in Sheffield.
Please note
If your pregnancy tissue result confirms that you had a normal pregnancy then you do not need further follow up.
Follow up with Specialist Centre: Trophoblastic Screening and Treatment Centre, Sheffield
We can only say you have had a molar pregnancy after it has been tested in the laboratory.
If the lab confirms that you have had a molar pregnancy you will be referred to the Trophoblastic Screening and Treatment Centre in Weston Park Hospital in Sheffield. They will contact you and you will be followed up by their doctors for at least six months.
This follow-up involves measuring the pregnancy hormone (hCG) either through urine or blood tests or both until the hormone level fall to non pregnant levels. Fortunately, you don’t usually need to travel to Sheffield for this follow up. The centre will post you the pack for the tests with information on what to do at home. You will need to go to either your GP surgery or local hospital to get blood tests done. You can collect your urine (wee) sample at home.
It is important that you are followed up until your hCG hormone level falls to normal. If it does not fall to normal you may be offered further treatment through the specialist centre.
Why is follow up important?
It is important that you do not get pregnant for at least six months after your pregnancy hormone levels have returned to normal. This may seem extremely frustrating especially if you are keen to conceive again.
However, it is extremely important not to get pregnant for two reasons:
- To increase your chances of being completely recovered. Follow up means that there is a recovery rate of 98-100%.
- To reduce the chance of the molar pregnancy progressing to gestational trophoblastic neoplasia (GTN).
Follow up at St James’s University Hospital, Leeds
You will be followed up in clinic by gynaecology doctors at St James’s University Hospital. The first appointment is within 4-6 weeks of receiving your diagnosis and the second is normally three months later. These appointments are usually over the phone. Occasionally, a face to face appointment is offered.
What happens if my pregnancy hormone levels don’t fall?
If you have a complete molar pregnancy, there is a one in 20 chance of needing further investigations and possibly chemotherapy.
What is gestational trophoblastic neoplasia (GTN)?
GTN is a rare form of cancer. It has a cure rate of over 99% if it develops after a molar pregnancy. It occurs when some of the molar pregnancy tissue persists. It is usually diagnosed if your HCG levels do not return to normal which is why follow-up is so important.
GTN can also occur after a normally progressing pregnancy or miscarriage but this is much rarer.
If you continue to bleed after a miscarriage or birth you should do a pregnancy test and see your GP if it is positive.
If you are diagnosed with GTN you can get more information from Weston Park Hospital, Sheffield.
When is it safe to start having sex again?
When you feel emotionally ready you can safely have sexual intercourse when any vaginal bleeding or discharge has stopped.
However, if you are feeling tired or sore or are still in pain you may wish to wait longer.
Please note
It is extremely important you do not get pregnant again until your follow up is finished. If you do become pregnant you are at a higher risk of having another molar pregnancy.
What contraception can you use?
After a molar pregnancy it is important you use contraceptives such as condoms; the combined oral contraceptive pill or the implant. Your Dr or GP will be able to discuss this with you.
Pregnancy after Molar Pregnancy
Having a molar pregnancy does not affect your chances of having another baby. You should not get pregnant until your follow-up programme is complete. It is usual for follow-up to last at least 6 months.
The risk of a molar pregnancy happening again is low. If you had a partial molar pregnancy you have less than a 1% chance of having a molar pregnancy.
Pregnancy after Gestational Trophoblastic Neoplasia (GTN)
Your periods usually stop if you have chemotherapy for GTN. However, they should restart a few weeks to months after completing chemotherapy. More than 80% of women following chemotherapy for GTN will have another pregnancy.
If you need high dose chemotherapy treatment for your GTN, your fertility may not return after chemotherapy. Fortunately, very few women need high dose chemotherapy.
You are advised not to get pregnant for 12 months after treatment is complete if you are treated with chemotherapy.
It is important to take the advice given to you by the specialist centre.
Emotional recovery
Everyone deals differently following a molar pregnancy.
You may feel some of the following;
- Upset or fear over the experience.
- Worry about getting pregnant again.
- Grief or shock.
- Guilt or blame over what has happened.
Please feel free to talk about these concerns to the doctors and nurses on the gynaecology assessment and treatment unit, your GP or the Miscarriage Association who also deal with women who have had a molar pregnancy.