The two main types of lung cancer are called non-small cell and small cell.
Often, those with lung cancer also have other chest disorders. Please follow this link to the Leeds Centre for Respiratory Medicine.
Potential treatment options may include:
- Surgery
- Drug therapy
- Radiotherapy
- Symptom management
- Or a combination of these options.
When treatment is complete
When treatment is complete a member of the team will discuss what happens next.
The Lung Cancer Nurse Specialist team are available for advice and can be contacted on 0113 2067916 or [email protected].
Surgery
Surgery is always considered if the lung cancer can be removed in its entirety. The main factors involved when considering if surgery is a suitable treatment option include:
- Whether the cancer can be completely removed
- Whether someone is fit enough to cope with surgery
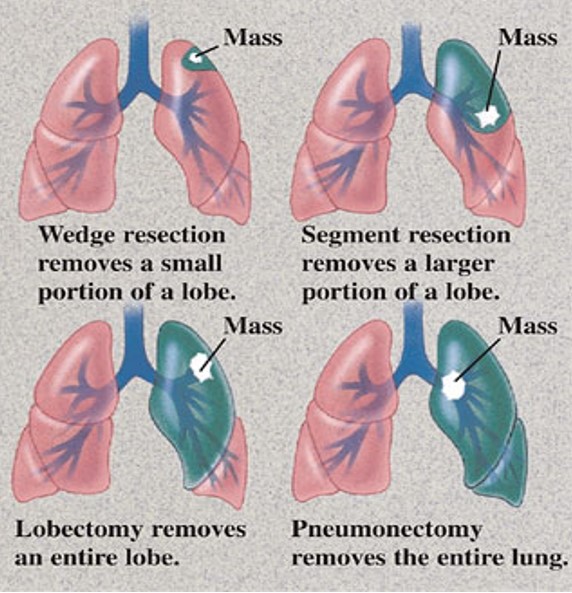
There are 4 common surgical procedures to remove lung cancer and include
- Wedge resection – the removal of abnormal tissue from a lobe of the lung
- Segmental resection – the removal of a larger portion than a wedge
- Lobectomy – the removal of a whole lobe of the lung
- Pneumonectomy – the removal of an entire lung
The techniques used to do the above procedures include:
Video Assisted Thoracoscopic Surgery (VATS)
This is also known as ‘Keyhole’ surgery. It is a minimally invasive surgical procedure used to access inside the chest area. During the procedure 2 to 3 small cuts, about 2cm long will be made. This allows the surgeon to pass a tiny camera (thoracoscope) into the chest area to watch their progress on a screen. The surgeon then uses the other two small cuts to pass the surgical instruments into the chest area.
Robotic-Assisted Thoracoscopic Surgery
This is a minimally invasive procedure used to access the chest cavity. The procedure is done under a general anaesthetic. During Robotic-Assisted Surgery the surgeon makes 5 small cuts about 1 to 2cm long. These are used to insert the surgical instruments, which are then connected to the arms of the robotic machine. The surgeon sits at a console near the patient where he controls the arms of the robot, which bend and rotate. The surgeon uses a 3D screen which provides a magnified view inside the chest.
Thoracotomy (Open)
In cases where keyhole/robotic surgery is not possible a Thoracotomy is done, this means there is just one longer cut made under the shoulder blade between 2 ribs. The 2 ribs are then parted to get access to the lungs.
All patients who are due to undergo a lung resection will be invited to attend a Patient Education Programme (PEP) session which covers:
- What to expect during your hospital stay
- Exercise and managing breathlessness
- Pain management
- Diet and managing poor appetite
- What happens after surgery
Related patient information leaflets
Drug therapy
The different types of drug therapy that can be used to treat lung cancer include: .
- Chemotherapy
- Targeted therapy
- Immunotherapy
The aims of these treatments are to:
- Shrink the cancer
- Keep the disease under control
- Help to manage symptoms
Please click on this link to find out more information on the chemotherapy page within the Leeds Cancer Centre.
Chemotherapy
Chemotherapy can be given either on its own, at the same time as radiotherapy, or it may be given before or after surgery. The chemotherapy regime will differ depending on the type of lung cancer that needs treating.
Patients with different types of lung cancer are likely to receive different combinations of chemotherapy. The oncologist will determine which is the most suitable regime.
How is chemotherapy given?
Chemotherapy can be given either by an intravenous infusion or in tablet form (only with certain drugs). Treatment is given in ‘courses‘, usually at three weekly intervals. You will usually receive all your chemotherapy treatments as an outpatient.
What are the side effects?
Detailed information will be provided about the specific side-effects and how to manage them before starting treatment with the most common side-effects being:
- Fatigue
- A drop in the blood count
- Nausea
- Hair loss (only with some chemotherapy drugs).
Chemotherapy drugs
The most common chemotherapy drugs used for the treatment of lung cancer include:
Immunotherapy
Immunotherapy targets specific parts of cancer cells to prevent growth. These treatments can include a group of drugs called:
- PDL1 inhibitors and include the drug Pembrolizimab
Detailed is given about side effects and how to manage them before starting treatment with the most common side effects being:
- Fatigue
- Immune system dysfunction (with PDL1 inhibitors)
Targeted therapy
EGFR inhibitors and include the drugs Gefitinib, Afatanib and Erlotinib (given as tablets)
Detailed is given about side effects and how to manage them before starting treatment with the most common side effects being:
- Fatigue
- Skin rash (with EGFR inhibitors)
Please click on this link to help with the management of side effects from Erlotinib.
Radiotherapy
Radiotherapy is the treatment of cancer with X-rays to kill cancer cells. It is often used on its own to treat lung cancer but it may also be given together with or after chemotherapy or surgery.
Radiotherapy is given as an outpatient with the treatment schedule varying in the number of treatments given.
The different radiotherapy schedules can include:
- Stereotactic radiotherapy
- Concurrent radiotherapy given with chemotherapy
- Radical radiotherapy
- High dose palliative radiotherapy
- Palliative radiotherapy
- Whole brain radiotherapy
- Prophylactic cranial radiotherapy
The oncologist always discusses the appropriate schedule including the planning process prior to the delivery of treatment. The lung cancer nurse specialist is also available to discuss the treatment and possible side effects.
Potential side-effects
Radiotherapy itself is painless. However, there are some side-effects associated with it and include fatigue, skin reactions, a sore gullet and occasionally breathlessness and cough. The side-effects usually gradually disappear after completion of treatment.
If you develop any side-effects, you should seek advice from your oncologist or lung cancer nurse specialist.