What is endometriosis?
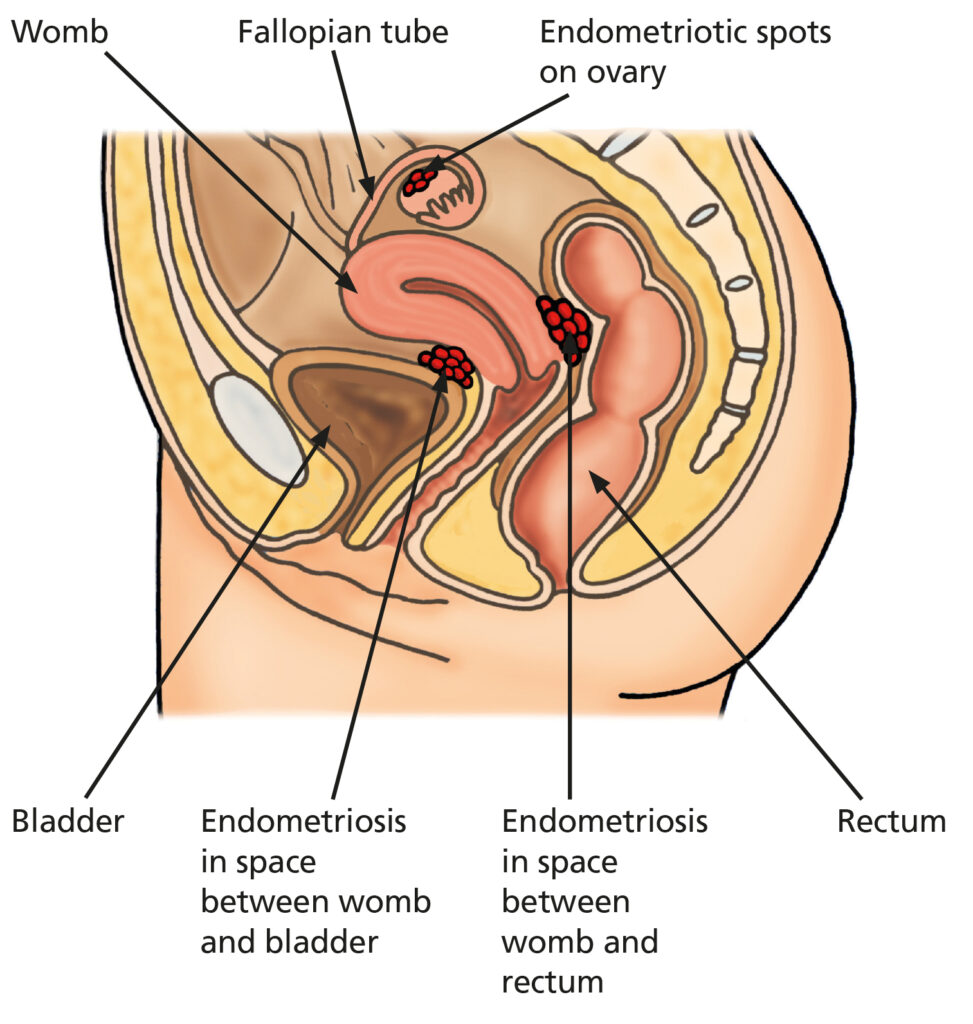
Endometriosis is a condition where endometrium like tissue, which is normally found in the inner part (the endometrium) of the womb (uterus), grows outside the womb, most commonly in the pelvis (the lower part of your tummy / abdomen). It is not known why the endometriosis grows in the wrong place.
Endometriosis tissue can implant anywhere in the pelvis, most commonly it is found on the ligaments that support the uterus (the uterosacral ligaments) or on the ovaries. Other places endometriosis can implant include on the bowel, bladder or the top of the vagina affecting their function. Sometimes endometriosis can be found within the muscle of the uterus (adenomyosis). Rarely endometriosis can be found in surgical scars or elsewhere in the body such as the diaphragm (muscle that helps you breathe).
About 10% of women or those assigned female at birth of childbearing age are affected by endometriosis. It is more likely to affect you if your mum or siblings have it. It can take many years to get a diagnosis and it can be a long-term condition that can have a significant impact on your physical and mental wellbeing.
What are the symptoms?
Some of the symptoms attributed to endometriosis can overlap with other conditions but the most common symptom of endometriosis is pelvic pain:
- Pain before a period starts
- Pain during periods (dysmenorrhea)
- Pain during or after intercourse (dyspareunia)
Other symptoms caused by endometriosis:
- Irregular or heavy periods (menorrhagia)
- Pelvic pain on opening bowels (in rarer cases where the bowel is involved) (dyschesia)
- Pelvic pain on passing urine (in rarer cases where the bladder is involved) (dysuria)
- Referred pain to the tops of the legs or back
- Fatigue
- Difficulty getting pregnant (subfertility)
Less commonly, endometrial tissue and adhesions attach to the bowel or bladder causing abdominal swelling, bleeding from the rectum (back passage) during menstruation or bowel obstruction.
Pelvic pain can come and go in a regular pattern or may be constant.
The severity of the pain and other symptoms of endometriosis can vary greatly; some patients with extensive endometriosis have no symptoms, whereas others with minimal disease have severe symptoms. This fact makes endometriosis very difficult to diagnose and treat.
Often, people will not start to have period pain from their endometriosis until it is already well established over several years.
How does endometriosis produce symptoms?
The exact cause of endometriosis is not known but it seems to be an inflammatory process regulated by hormones.
In a regular menstrual cycle the lining of the womb thickens and later bleeds as a period in response to oestrogen made by the ovaries. In the same way endometriosis grows and bleeds in response to the oestrogen. This growth of endometriosis and bleeding can cause damage and inflammation to the surrounding tissues which causes pain. As the tissues heal scarring can form (adhesions) which can stick down normally freely moving organs such as the ovaries, bowel and bladder which can cause pulling of internal lining (peritoneum) and chronic pain.
Damage to the ovaries and fallopian tubes can contribute to subfertility but most patients with endometriosis will conceive naturally.
Endometriosis on the ovaries can form cysts containing old blood called endometriomas (also known as chocolate cysts). These cysts may cause pain as they increase in size, or if the old blood leaks. Occasionally the ovary containing the cyst can twist on the stalk that connects it to the womb causing pain. This is called ovarian torsion which may require emergency surgery to save the ovary.
How is endometriosis diagnosed?
Endometriosis can be a difficult condition to diagnose because the symptoms vary in different patients, are common and can mimic other conditions such as irritable bowel syndrome (IBS), painful bladder syndrome or pelvic inflammatory disease (PID). It takes 8 years on average to diagnose endometriosis.
Endometriosis can be diagnosed in a number of ways. Traditionally a keyhole surgery (laparoscopy) where endometriosis has been seen and or biopsied has been considered the best way to confirm a diagnosis of endometriosis. However, endometriosis can be sometimes seen on ultrasound scan or MRI (see section below).
Based on your signs and symptoms the diagnosis of endometriosis can be often assumed and treatment started based accordingly.
Further tests we offer
There are no blood tests used in the clinic to diagnose endometriosis.
- Ultrasound scan images the womb and ovaries, particularly looking for endometriomas (endometriosis cysts on the ovary), but small areas of endometriosis cannot be seen. Ultrasound can be suggestive of endometriosis e.g. if an ovary is stuck down or in an abnormal position. An ultrasound will be offered to most patients if this has not been performed recently. A normal ultrasound doesn’t exclude (rule out) endometriosis.
- Laparoscopy is a keyhole surgery performed under general anaesthetic. A camera and surgical instruments are placed through small holes in the abdomen to look in the pelvis for endometriosis and scar tissue which could be causing the symptoms. Extensive adhesions, lumps of endometriosis tissue (nodules) and endometriomas (endometriosis cysts on the ovaries) can also be seen. At laparoscopy, biopsies can be taken to be looked at in the lab to confirm the diagnosis. Mild to moderate endometriosis can be treated during the laparoscopy. However, a laparoscopy does not need to be a first line treatment and some patients can be successfully treated without surgery.
- MRI scan is sometimes offered prior to surgery if advanced/deep endometriosis is suspected.
- Other tests include a camera to look into the bowel (sigmoidoscopy / colonoscopy) or the bladder (cystoscopy) which are sometimes arranged when looking for deep endometriosis.
How does endometriosis progress?
The natural cause of endometriosis is currently unknown. The available limited evidence from research studies suggest that endometriosis may get better in 3 out of 10 patients; become worse in 3 out of 10 patients; whilst remain unchanged in the remaining patients without treatment to their endometriosis.
At present there are no curative treatment for endometriosis or associated symptoms, and when offering treatments to patients with endometriosis, doctors cannot predict who are likely to have their endometriosis worsened if untreated.
Even with treatment, endometriosis can recur, but some patients with severe untreated endometriosis may be at risk of complications such as obstruction or blockage of the ureter (the tube between the kidney and bladder). These issues need to be considered when choosing the treatment options.
Endometriosis and Fertility
The relationship between endometriosis and fertility is not yet fully established or understood. There are many individuals with endometriosis who become pregnant without difficulty but endometriosis is found in 1 in 4 patients who are undergoing investigations such as a laparoscopy for subfertility investigation (Cochrane 2002).
There are no preventative surgical treatments that have shown to be effective to improve future fertility, yet for those patients who are having difficulties in getting pregnant; consultation with an infertility expert is initially needed for particular advice for treatment for endometriosis. Endometriosis services in Leeds work closely with a fertility experts in Leeds Fertility Unit to guide treatment of the endometriosis.
Why and how is endometriosis staged?
The stage of your endometriosis refers to how severe your endometriosis is. It is graded from stage 1 (a small amount of endometriosis) to stage 4 (the severest form of endometriosis).
In the UK staging of endometriosis isn’t recommended as the stage (or visual severity) of endometriosis often doesn’t reflect the severity of a patient’s symptoms.
We aim to offer treatments based on patients’ symptoms, preferences and priorities rather than the stage of disease. That being said, the amount of the endometriosis tissue present in the pelvis can be described by doctors in a certain way using the classification provided by the American Society for Reproductive Medicine to assess the severity and extent of the disease. This system gives points based on where the endometriosis tissue is and how deep beneath the surface it extends to, so it can assist in staging the extent of endometriosis.

How is Endometriosis treated?
There is no cure for endometriosis. The aim is to improve your quality of life by individualising the treatment to your symptoms, preferences and priorities. This can be done in a number of different ways, sometimes combining treatments. The main categories are: complementary therapies (including lifestyle changes), pain medications, hormonal medications and/or surgery.
Complementary therapies and lifestyle
- Self-care action plan: Stress may make the pain and fatigue associated with endometriosis worse. Patients with endometriosis often find some form of relaxation therapy useful such as exercise, yoga, meditation or the Alexander Technique. We would encourage patients to look at joining the Endometriosis UK online community or support groups. To this end some patients would benefit from psychological support therapies and or counselling.
- Acupuncture: There have been trials that have demonstrated a benefit for some patients with endometriosis undergoing acupuncture, however the overall quality of this evidence and their trials was poor. Acupuncture is safe and if it works for you it would avoid other forms of therapy.
- CBD oil (full spectrum): CBD is a derivative from the cannabis plant and acts on CBD pain receptors in the body. CBD oil is legal in the UK and available to buy online. There was a large study in Canada asking patients with endometriosis what alternatives they had tried to help with pain and how successful it had been. CBD oils and acupuncture were the top two most successful.
- Diet modifications: Some patients with endometriosis have bowel related pain and or abnormal function. Sometimes this can be related to an intolerance such as Gluten or Lactose, which are common in the general population, and can worsen some symptoms that have been put down to endometriosis. Excluding these from your diet can be helpful to see if that makes a difference to your symptoms. We have had patients who have researched diets specific to endometriosis and feel that this change alone improved their symptoms. There is currently no evidence to support this practice but as long as it is safe and balanced it could work for some patients.
- IBS (Irritable bowel syndrome) and Endometriosis: There is a recognised overlap with IBS or Functional bowel symptoms and endometriosis. In a recent survey approximately 60% of patients diagnosed with endometriosis had functional bowel symptoms, in particular bloating, pain and change in stool frequency and consistency.
- There is some emerging evidence that patients with endometriosis and functional bowel symptoms may benefit from the FODMAP diet.
When bloating is the predominate symptom, this is usually due to an imbalance of abdominal to diaphragmatic breathing (also known as abdominophrenic dyssynergia). MRI scans have been performed on patients who experience bloating ‘I look pregnant’ and found that their bowel isn’t in fact full of gas.
There is an excellent YouTube video from the University of Michigan that goes through diaphragmatic breathing in more detail:
Hyoscine butylbromide (also known as Buscopan) is an antispasmodic drug that has been shown to help with the pain associated with IBS / functional bowel problems, and this can be purchased over the counter. We often recommend taking peppermint concentrate daily as this has been useful for some patients. These can be purchased over the counter as Colpermin or from shops like Holland and Barrett or Amazon if you have IBS rather than endometriosis, your GP is the best initial contact.
Normal abdominal accommodation

In normal conditions, the abdominal walls adapt to its content. A volume increase elicits a coordinated abdominophrenic response to prevent distension.
Abdominophrenic dssyneria

Abdominal distension is produced by a paradoxical contraction of the diaphragm and anterior wall relaxation.
Other things that our patients have tried with varying degrees of success to help reduce pain and improve their quality of life are:
- Reflexology
- Transcutaneous electrical nerve stimulation (TENS)
- Vitamin B1 and magnesium supplements
Pain relief medications
We advise starting with simple over the counter pain relief such as paracetamol and non-steroidal medications such as ibuprofen. Studies show non-steroidal medications alone can reduce pain by up to 50% because they target inflammatory conditions like endometriosis. If required prescription pain relief can be tried and in severe cases advice can be sought from pain medicine specialists. We often recommend trying to avoid the category of pain relief called opiates long term as these can become addictive and cause side effects such as chronic constipation and paradoxically worsening pain.
Often when some patients have lived with pain for a long time their body experiences pain in an abnormal and exaggerated way. Pain modulators such as Amitriptyline can be used to try and restore how your body should experience pain as well as reducing the amount of pain you experience.
Hormonal medical treatment
We know when the ovaries are not functioning and not producing oestrogen, endometriosis symptoms improve. Naturally in life the ovaries are not working before puberty, and they stop in pregnancy and after the menopause. Hormonal medical treatments are used to temporarily stop the ovaries making oestrogen.
Traditional contraceptive medications are the first line hormonal treatments. These include combined contraceptive pills (containing oestrogen and progesterone), mini pills (progesterone only pill), injections, implants and intrauterine coils (such as Mirena and Benelixa).
There is no strong evidence that any contraceptive is superior to any other in treating pain, however they work in different ways and some have additional benefits such as effects on improving heavy periods. The doctor will discuss each option with you to find the most suitable option for you. More information can be found at the NICE guideline patient decision aid Hormone contraceptives for endometriosis symptoms PDS (nice.org.uk). Whichever option is tried, it is recommend to use the treatment for at least 3-6 months to assess the effect the treatment has on symptoms. If symptoms have improved on treatment, there may be no need for any additional treatments.
Dienogest is an endometriosis specific pill that contains a progesterone licenced to treat the pain associated with endometriosis. It has been found to be very effective in improving pain as well as reducing the size of endometriomas (chocolate cysts) and delaying the recurrence of endometriosis after surgery. It also comes with a low side effect profile. In the studies the main reason patients stopped taking Dienogest was headache 0.4% or 1 in 250.
Second / third line treatment is called Gonadotrophin releasing hormones (GNRH). These come in injection or nasal spray form. They cause a temporary menopause state by stopping the ovaries from functioning. Your ovaries will begin to function once this treatment is stopped unless you have gone through the natural menopause. Hormone replacement therapy (HRT) is usually given at the same time to prevent symptoms of the menopause. The length a patient can be on these injections can vary and is usually dictated by the patients symptoms, preferences and priorities.
Surgical treatment
Laparoscopy (keyhole surgery) can be used to diagnose and treat endometriosis. At the time of surgery endometriosis and scar tissue can be removed by cutting it away or destroying it with heat.
The studies conducted for the surgical management of endometriosis are of low quality and it can be hard to work out if and who will benefit the from surgery and for how long. There are currently trials underway to explore these issues. If you undergo surgery for endometriosis and are not trying to fall pregnant immediately after, we recommend some hormonal therapy to go along side your surgery such as the Mirena coil, Dienogest or GnRH.
Laparoscopic treatment can improve pain in a significant number of patients. Combining the surgery with a contraceptive can improve symptoms further and keep symptoms away for a longer period of time.
Occasionally, patients are found to have more complex endometriosis than expected prior to laparoscopy.
If this is the case full treatment will not be performed at the time because the risks associated with surgery are increased. Your understanding of these risks is required before proceeding with major surgery.
After your procedure, you would be informed of the findings and another appointment would be made, possibly with a follow up scan. Patients with complex endometriosis usually require input of more specialities such as fertility medicine, colorectal surgery, urology surgery, plastic surgery and or thoracic surgery. Patients requiring considerable input from other specialties will be discussed at a multidisciplinary team meeting to make sure that we are offering you the correct treatment for your symptoms, preferences and priorities.
As a last resort removal of the uterus, cervix, fallopian tubes and ovaries (hysterectomy and bilateral salpingo-oophorectomy – for more information on this procedure please see the separate patient leaflet) may be offered. This is usually reserved for people who have completed their family and is often a technically difficult procedure. Hysterectomy alone (without removal of the ovaries) leads to a 40% recurrence of endometriosis after 5 years but it’s an effective treatment for adenomyosis. Surgical removal of both ovaries can prevent endometriosis from recurring in up to 90-95%, your doctor will explain the risks and benefits of having your ovaries removed. Afterwards, hormone replacement therapy with oestrogen and progesterone can be offered depending on your age and the symptoms you experience. Having a combined preparation reduces the chances of endometriosis coming back.
Approximately a third of individuals who had improvement in symptoms from an initial operation will develop recurrence of symptoms later and may require further surgery. Repeated surgery for endometriosis excision is potentially riskier with increase possibility of serious complications.
Before any operation the surgeon will discuss the specific risks of the operation with you and any alternative treatments available. For more complex endometriosis surgery there is a separate patient information leaflet but for a standard endometriosis laparoscopy the main risks are:
- Temporary abdominal and shoulder tip pain.
- Bruising around the wounds and scarring.
- Infection occurs in up to 5% patients. Most commonly there are chest, urine or wound infections.
- Risk of significant bleeding or developing a hernia in one of the scars occurs in around 1% cases.
- A serious complication such as injury to bowel, bladder, ureter or blood vessels or needing a laparotomy (open surgery with a big cut) occurs in about 1:500 laparoscopies.
- Very rarely patients can develop life threatening blood clots or other complications.
- In up to half of patients undergoing laparoscopy for suspected endometriosis or pelvic pain no cause for their pain will be found or pain will continue despite treatment.