This booklet aims to provide you with information on:
- How you may feel following surgery
- Your recovery after the operation
- How to look after your wound
- Your follow up after the operation
After the operation:
When you wake up from the general anaesthetic you will be in the recovery room in the Geoffrey Giles theatres at St James’s Hospital. You will stay there for a couple of hours to make sure your condition is stable before you are transferred back to the ward. After having an anaesthetic you might wake up:
- With a sore throat
- Feeling slightly sick
- In pain or some discomfort
If you do experience any of these symptoms please let the nurse who is looking after you know so they can help you.
You will have a plastic mask over your nose and mouth to maintain good levels of oxygen and there will be a needle in your arm with fluid running to keep you hydrated until you are able to drink normally. You will also have a control button to administer pain relief as and when you need it.
This is called Patient Controlled Analgesia System (PCAS) and you will usually have it for up to 24 hours following surgery. You will also be given oral pain relief.
Occasionally donors need a urinary catheter in their bladder after surgery. You may also have a wound drain which is a plastic tube to allow fluid to escape from the space previously occupied by your kidney. Your surgeon will discuss this with you on the morning of your surgery.
While you are in the recovery room a nurse will check your blood pressure and pulse rate regularly. When you are well enough they will contact the ward staff and someone will come to the recovery room to take you back to the ward.
Ward visiting times are 14:00 to 16:00 and 18:00 – 20:00
J49 – 0113 20 69149
J50 – 0113 20 69150
J83 – 0113 20 69183
Please note we do not allow flowers on the ward due to the risk of infection.
You can start drinking as soon as you are fully awake and you do not feel too sick. This is usually two to three hours after you arrive on the ward post operatively.
If you can tolerate the fluids you can have something light to eat in the evening. You are encouraged to eat as it will allow you to take tablet painkillers in addition to the PCAS.
Later in the evening after your surgery you will be encouraged to sit in your chair for two hours and the day after your surgery you will be encouraged to get out of bed and start walking around the ward area. This will be uncomfortable to start with but it will improve the more you move about. This is important to help prevent any complications, such as a chest infection or deep vein thrombosis (DVT).
The surgery is performed using a laparoscopic (or keyhole) technique. You may feel bloated following the operation as during this procedure your abdomen is expanded with air. You may need to take laxatives for a couple of days after the operation to improve this feeling and to prevent constipation – using chewing gum for fifteen minutes four times a day can also help with this symptom.
As well as feeling bloated you may also experience some shoulder pain as the gas may irritate the diaphragm muscle which presents as pain in your shoulder. This can sometimes be relieved by walking and peppermint (i.e. in your tea).
What happens next?
You should go home when you are able to:
- Pass urine freely
- Move around without too much pain
- Eat without feeling sick
The best place for you to recover is in your own home with your own comforts. This is usually between one to two days following surgery.
You will be taught how to give yourself an injection which thins your blood to reduce the chance of you getting a DVT. You will receive a total of seven injections. This is a small injection, but if you do not want to do it yourself we could teach a family member, or arrange for your practice nurse to give it.
You will need to wear your TED (anti thrombus) stockings for the duration of your inpatient stay. It is important that you continue to be mobile at home to reduce risk of DVT.
You will be discharged home with pain relief medication and you are advised to take these as long as needed. The renal pharmacist will come to see you before you go home and they will discuss your discharge medications with you.
Wound Care and after care advice:
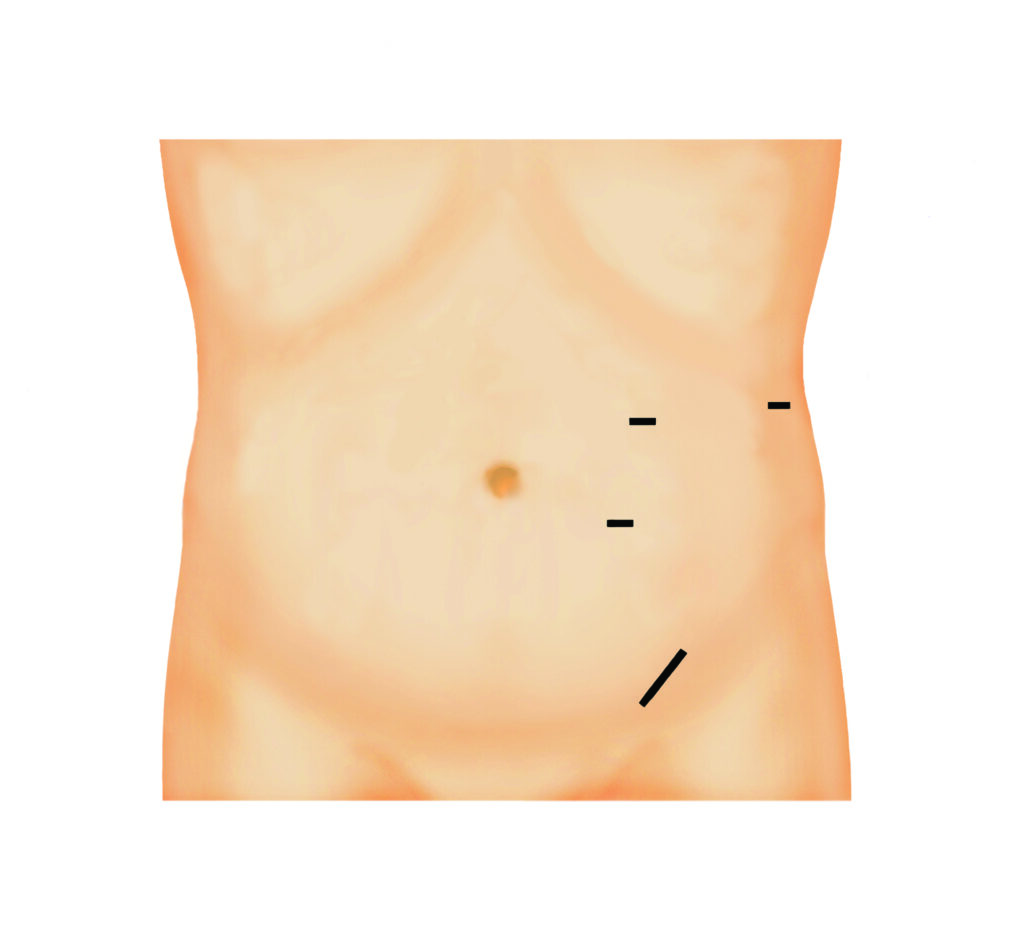
You will have three small cuts on your abdomen from the keyhole surgery and one slightly longer incision just above your groin from where the kidney was removed. These cuts are closed with dissolvable stitches.
- You will be given some spare dressings to take home. You can shower with your dressings on, you will need to remove them after your shower and replace them with clean ones if needed. If your wound is clean and dry you do not need to cover it with dressings. It is not advisable for you to soak in the bath until your wounds are completely healed (usually two weeks).
- If you notice any redness or swelling around your wound area please contact the renal live donor team as your wound will need to be reviewed.
We advise that you avoid heavy lifting or strenuous physical activities for at least six weeks following surgery i.e. lifting shopping bags/children, heavy gardening. This could increase your risk of developing a hernia.
You should wait four weeks following surgery before returning to physical exercise (i.e. light gym training/swimming). You can then gradually increase your physical activity. We advise that you avoid returning to driving for four to six weeks following surgery, you must be confident that you can safely perform an emergency stop.
When you return to work depends on the type of job that you do and your recovery progress, again this is usually four to six weeks following surgery.
It is not uncommon that you may feel low in mood after surgery, this can be due to the emotional ‘rollercoaster’ you have been through and it usually only lasts for a couple of days. Some donors may feel a sense of anti-climax after discharge as the medical team transfer their attention towards the care of the recipient. You can contact the transplant co-ordinators at any time should you feel concerned about your recovery.
In men who donate their left kidney it is possible that there may be some testicular discomfort or swelling. This usually resolves without intervention but if you are concerned please do not hesitate to contact us.
Follow up
Once discharged from hospital the live renal donor team will telephone you. You will then receive an appointment with the consultant surgeon who performed your operation approximately six weeks after donation to check that you have recovered and your wound is healing.
In the long term you will be reviewed for an annual general health check. This will involve a weight and blood pressure check as well as taking blood and urine samples. You can get these done at your GP, we will post the request cards out to you and follow up with a telephone consultation.
Some painkillers, which belong to a group of drugs called NSAIDs (Non-Steroidal Anti-Inflammatory Drugs) may be harmful to the kidneys with prolonged use. After your nephrectomy we advise that you do not take these drugs for prolonged periods. If you do require long term treatment then your GP should find an alternative. Examples of NSAID’S include ibuprofen (Neurofen), diclofenac, naproxen.
Suggestions from other donors
- Remember on the journey home to try to avoid all speed bumps.
- For discharge you may want to bring some loose clothing as you will feel bloated.
- Take it easy, don’t rush yourself (but stay active) and enjoy the time off work.
- Make small changes to help make things easier for you when you first get home i.e. make sure everything you need is close to hand, have someone to help you with heavy lifting, make sure you have somewhere comfortable to sit and relax.
The Leeds transplant team would like to take this opportunity to thank you very much for your donation, this is a very generous gift.
Online
www.leedsth.nhs.uk/a-z-of-services/kidney-transplantation/
Outside of working hours
Please contact either Ward J49 (0113 206 9149) or Ward J50 (0113 206 9150)